 “Dysregulation in neutrophil biology and the formation of neutrophil extracellular traps (NETs) may play a prominent role in the initiation and perpetuation of a number of systemic autoimmune diseases, including systemic lupus erythematosus (SLE) and rheumatoid arthritis,” says Mariana J. Kaplan, MD, a distinguished investigator in the systemic autoimmunity branch of the National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health, Bethesda, Md.
“Dysregulation in neutrophil biology and the formation of neutrophil extracellular traps (NETs) may play a prominent role in the initiation and perpetuation of a number of systemic autoimmune diseases, including systemic lupus erythematosus (SLE) and rheumatoid arthritis,” says Mariana J. Kaplan, MD, a distinguished investigator in the systemic autoimmunity branch of the National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health, Bethesda, Md.
Dr. Kaplan is the author of a review that is part of a series on immunology for rheumatologists launched earlier this year in Arthritis & Rheumatology (A&R).1 In this new installment, Dr. Kaplan explores the role of NETs in SLE.2
The comprehensive review builds on a case study demonstrating the clinical manifestations of SLE while exploring the role of NETs in the pathogenesis, diagnosis and treatment of SLE. Dr. Kaplan refers to the case study throughout the review, which includes many references, along with a detailed figure demonstrating the mechanisms by which NETs promote autoimmunity and organ damage in SLE.

Dr. Kaplan
“Current evidence supports a role for neutrophil subsets and NETs in organ complications and in the development of premature cardiovascular disease,” says Dr. Kaplan.
Case Study
The case study follows a 31-year-old woman patient presenting with a six-month history of fatigue, joint pain, intermittent fevers and a rash exacerbated by the sun. She first noticed the symptoms following an upper respiratory tract infection six months earlier. The patient also reported non-painful, recurrent mouth ulcers, Raynaud’s phenomenon and hair loss for the past three months. Her symptoms persisted despite taking acetaminophen and avoiding sun exposure.
A physical examination showed a red, macular malar rash, sparing the nasolabial folds, a maculopapular rash on her upper arms, oral ulcers, and swelling and tenderness in her knees and multiple joints in her hands and feet.
Laboratory tests indicated leukopenia; lymphopenia; mild neutropenia; an elevated erythrocyte sedimentation rate; normal C-reactive protein levels; increased levels of anti-nuclear antibodies, anti-double-stranded DNA and anti-Ro antibodies; and decreased C3 and C4 levels.
Renal function test results were normal, with no proteinuria. Other findings included low high-density lipoprotein; elevated low-density lipoprotein and total cholesterol; bilateral increased carotid intimal media thickness; an impaired cholesterol efflux capacity; elevated myeloperoxidase (MPO):DNA remnants and citrullinated histone H3:DNA remnants consistent with NETs and the presence of low-density granulocytes (LDGs).
“Given the clinical presentation and laboratory findings, you diagnose the patient with SLE and pre-clinical atherosclerosis and dyslipidemia, and initiate an antimalarial, a statin and low-dose prednisone, as well as advising her regarding sun protection, vitamin D intake, warranted vaccinations and other general preventive measures for SLE comorbidities,” Dr. Kaplan writes.
NETs
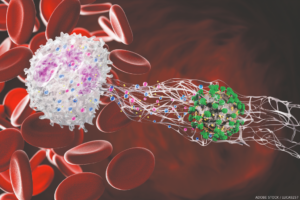
The article reviews research findings on neutrophil dysregulation and NETs in SLE; the formation of NETs, including the unique form of cell death, NETosis; LDGs and vascular damage in SLE; NETs and autoantigen exposure; impaired NET clearance; and the link between NETs and inflammation and organ damage.
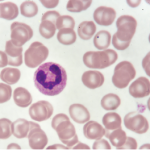
NETs are web-like structures comprising DNA, RNA, histones and anti-microbial proteins, “which are released to the extracellular space by activated neutrophils in response to a variety of microbial and sterile inflammatory stimuli,” Dr. Kaplan explains.
In SLE, the dysregulated formation and impaired clearance of NETs lead to their “accumulation within tissues and to their extended half-life in circulation, potentially contributing to perpetuating autoantigen generation and modification, inflammation and tissue damage,” Dr. Kaplan writes. “NETs may contribute to the pathogenesis of lupus nephritis, lupus-associated skin disease, thrombosis, vascular damage and tissue injury in various organs, including pregnancy complications, such as preeclampsia.”
When exposed to modified autoantigens, NETs may trigger the production of autoantibodies, including anti-double-stranded DNA and anti-nucleosome antibodies, “perpetuating the autoimmune responses in SLE,” Dr. Kaplan continues. NETs promote plasmacytoid dendritic cell activation in vitro and type I interferon (IFN) production, “driving systemic inflammation and amplifying immune dysregulation” in SLE.
NET Biomarkers
Elevated NET levels and LDGs have been linked to increased disease activity in patients with SLE. Measuring markers for NETs and LDGs may help diagnose and monitor disease activity, delivering insights into disease progression and treatment response.
Markers that identify NETs—detected in blood and tissue samples via several methods—include citrullinated histone-DNA complexes, DNA-MPO or DNA-neutrophil and elastase complexes. However, the use of cell-free DNA should be avoided as a sole marker because it is not a specific indicator of NET formation.
“Once properly validated, monitoring NET levels could provide valuable information for assessing disease progression and treatment response, “Dr. Kaplan writes. “NETs could be used to identify patients at risk of relapse and guide preemptive therapeutic interventions. Further, anti-NET antibodies targeting NET components, such as citrullinated histones and MPO, have emerged as potential biomarkers for lupus diagnosis and stratification,” and “studies have linked levels of LDGs to vascular damage.”
In the case study, the patient’s active disease was associated with the presence of elevated NETS and LDGs. “It is possible that these NETs have contributed to her active skin and joint disease, although tissue biopsies would have been needed to document their involvement,” Dr. Kaplan explains.
The accelerated vascular damage and dysregulated lipoprotein panel were potentially triggered by LDGs and NET formation. “[Although] NETs and LDGs are not currently used as clinical biomarkers of vascular risk, it is possible that they will be incorporated in the future in the clinical decision management in SLE patients,” she adds.
Therapeutic Avenues
New therapeutic avenues to mitigate harmful effects of NETs in SLE include “targeting NET formation, promoting NET clearance or neutralizing NET components,” Dr. Kaplan writes.
SLE therapies that potentially reduce NET formation, number and the harmful effects of NETs include hydroxychloroquine; tofacitinib, a Janus kinase inhibitor; some anti-B cell therapies; and the type I IFN receptor blocker, anifrolumab.
“By elucidating the mechanisms underlying NET-mediated inflammation, clinicians can develop targeted therapies to mitigate disease activity and improve outcomes in lupus patients,” Dr. Kaplan writes.
Investigational agents targeting NETs include PAD4 inhibitors, preventing histone citrullination and NET formation; NADPH oxidase and/or mitochondrial reactive oxygen species (ROS) inhibitors, preventing NETosis; DNase therapy, reducing the pro-inflammatory effects of NETs by degrading their DNA; and anti-IFN therapy, reducing NET-induced inflammation and autoimmunity.
“Further research is needed to validate the diagnostic and therapeutic utility of NET-targeted interventions and optimize their integration into clinical practice,” Dr. Kaplan concludes.
Katie Robinson is a medical writer based in New York.
References
- Bucala R, Solomon DH. Immunology for the rheumatologist: Arthritis & Rheumatology introduces a new problem-based immunology review series with great educational potential. Arthritis Rheumatol. 2024. Jan;76(1):9–10.
- Kaplan MJ. Exploring the role of neutrophil extracellular traps (NETs) in SLE: A clinical case study and comprehensive review. Arthritis Rheumatol. 2024;76.