ACR Convergence 2021—The world of vasculitis has seen several significant changes over the past year, and these important advances were discussed by Peter Merkel, MD, MPH, chief, Division of Rheumatology, University of Pennsylvania, Philadelphia, during the ACR Convergence 2021 annual Review Course.
ACR Convergence 2021—The world of vasculitis has seen several significant changes over the past year, and these important advances were discussed by Peter Merkel, MD, MPH, chief, Division of Rheumatology, University of Pennsylvania, Philadelphia, during the ACR Convergence 2021 annual Review Course.
Dr. Merkel began by noting that the ACR and Vasculitis Foundation worked together to publish guidelines this year for several forms of systemic vasculitis. Among these guidelines was a document dedicated to anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis, which can come in the form of granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA) or eosinophilic granulomatosis with polyangiitis (EGPA).
Treatments
Dr. Merkel noted that for non-severe ANCA-associated vasculitis (i.e., not organ- or life-threatening), methotrexate and rituximab both represent reasonable agents for induction of remission; maintenance medications can include methotrexate, azathioprine, rituximab or—as a third-line option—mycophenolate mofetil.
For severe disease, cyclophosphamide remains an option for induction of remission, but it is being used less and less in the U.S., given the efficacy demonstrated by rituximab and the significant toxicities that can occur with cyclophosphamide treatment.1
Avacopan may now help fulfill an unmet clinical need to reduce or avoid glucocorticoids while yielding better long-term outcomes for patients.
Remission Maintenance
Concerning maintenance of remission in ANCA-associated vasculitis, the MAINRITSAN-1 trial found that 500 mg of rituximab every six months is more effective than 2 mg/kg/day of azathioprine for remission maintenance.2
Dr. Merkel did point out several questions that remained after this trial was completed, including: What would the effects of a higher dose of rituximab have been? Because all patients in this study received cyclophosphamide for induction, what is the generalizability to patients who do not receive this agent for induction treatment? What would have been the results if azathioprine had not been tapered from the 2 mg/kg/day dose after one year?
Dr. Merkel also discussed the RITAZAREM trial, for which he is a co-primary investigator. This is a study of 190 patients with GPA or MPA with relapse treated with rituximab at a dose of 375 mg/m2 intravenous (IV) infusion weekly for four consecutive weeks. Patients who were then in remission at four months were randomized to either rituximab 1g IV every four months or azathioprine 2 mg/kg/day from months 4 to 24.
Dr. Merkel et al. found that rituximab was superior to azathioprine for preventing disease relapse, but he did point out in his talk that the rate of relapse accelerated in both arms once either agent (rituximab or azathioprine) was stopped at 24 months.3
In broadly discussing options for remission maintenance in patients who have achieved remission with rituximab as the induction agent, Dr. Merkel explained that rituximab 500 mg IV once every four to six months may be the most appropriate option for most patients. Methotrexate and azathioprine remain as potential alternatives, but trials like MAINRITSAN-1 and RITAZAREM should lead to caution with these medications given the increased risk of relapse.
Patients can be further stratified into high- and low-risk categories, and the finding that patients with new-onset, anti-myeloperoxidase antibody positive ANCA-associated vasculitis are at lower risk of relapse than those with other subtypes of ANCA-associated vasculitis indicates that a watch-and-wait approach after one course of rituximab or 18 months of cyclophosphamide followed by azathioprine may be appropriate in these patients.
Dr. Merkel noted that issues that may affect decisions on maintenance agents include cost, risks of infection associated with long-term treatment, and when and how to use low-dose glucocorticoids as part of remission maintenance.
Plasma Exchange
Dr. Merkel next talked about the PEXIVAS trial, for which he was also a co-primary investigator.4 Rates of end-stage renal disease (ESRD) and mortality continue to be high in ANCA-associated vasculitis, and plasma exchange has often been used in severely ill patients. Thus, PEXIVAS researchers sought to answer these questions: Does plasma exchange reduce death from any cause or ESRD? Is a reduced-dose oral glucocorticoid regimen non-inferior to a standard dose regimen in terms of death from any cause or ESRD, and is it superior in regard to serious infections?
In this randomized, controlled trial, Dr. Merkel et al. found no difference in mortality or ESRD rates in the group of patients that received plasma exchange and those who did not receive plasma exchange. Further, reduced-dose glucocorticoids were non-inferior to the standard-dose regimen in the primary and all secondary outcome measures, and 31% fewer serious infections occurred in the reduced-dose group than in the standard-dose group.
This second conclusion, and the results of other studies, such as the LoVAS trial, have created excitement about the potential for greatly reduced steroid doses in the treatment of many patients with ANCA-associated vasculitis.5
Avacopan
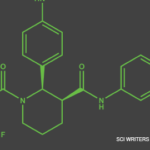
Adding to this excitement is the ADVOCATE trial, which looked at the C5a receptor inhibitor avacopan and compared this treatment to prednisone in patients with ANCA-associated vasculitis who were being treated with rituximab or cyclophosphamide/azathioprine. In this study, avacopan was found to reduce glucocorticoid use and toxicity by reducing the need for extended daily glucocorticoid therapy; it was also found to improve disease control and recovery of renal function.6
Following approval by the U.S. Food & Drug Administration in October 2021, avacopan may now help fulfill an unmet clinical need to reduce glucocorticoids while yielding better long-term outcomes for patients.
Jason Liebowitz, MD, completed his fellowship in rheumatology at Johns Hopkins University, Baltimore, where he also earned his medical degree. He is currently in practice with Skylands Medical Group, N.J.
References
- Chung SA, Langford CA, Maz M, et al. 2021 American College of Rheumatology/Vasculitis Foundation guideline for the management of antineutrophil cytoplasmic antibody-associated vasculitis. Arthritis Rheumatol. 2021 Aug;73(8):1366–1383.
- Guillevin L, Pagnoux C, Karras A, et al. Rituximab versus azathioprine for maintenance in ANCA-associated vasculitis. N Engl J Med. 2014 Nov 6;371(19):1771–1780.
- Smith R, Jayne D, Merkel P. A randomized, controlled trial of rituximab versus azathioprine after induction of remission with rituximab for patients with ANCA-associated vasculitis and relapsing disease [abstract]. Arthritis Rheumatol. 2019;71(suppl 10).
- Walsh M, Merkel P, Peh CA, et al. Plasma exchange and glucocorticoids in severe ANCA-associated vasculitis. N Engl J Med. 2020 Feb 13;382(7):622–631.
- Furuta S, Nakagomi D, Kobayashi Y, et al. Effect of reduced-dose vs high-dose glucocorticoids added to rituximab on remission induction in ANCA-associated vasculitis: A randomized clinical trial. JAMA. 2021 Jun 1;325(21):2178–2187.
- Jayne DRW, Merkel P, Schall TJ, et al. Avacopan for the treatment of ANCA-associated vasculitis. N Engl J Med. 2021 Feb 18;384(7):599–609