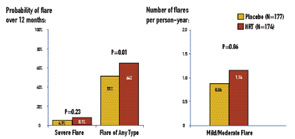
In contrast to severe flares, mild/moderate flares were significantly increased in the HRT arm: 1.14 flares per person-year for HRT and 0.86 for placebo (RR=1.34; P=0.01). The probability of any type of flare by 12 months was 0.64 for HRT and 0.51 for placebo (P=0.01). There was one death in the study, which occurred in the HRT group. There were three deep-vein thromboses (two on HRT and one on placebo), one stroke on HRT, and one thrombosis in an AV graft on HRT.
Mining Retrospective Data and Basic Science
Studies on the influence of past use of estrogens in the development of SLE have not yielded consistent results. (See Table 2) The concern and confusion regarding estrogen effects in SLE have led to studies of estrogen receptor expression in peripheral B cells of SLE patients. Overall, levels of estrogen receptors do not differ between SLE patients and non-autoimmune women. However, a variety of truncated estrogen receptor transcripts that can be produced. One study suggests that a short transcript encoding a constitutively activated estrogen receptor a may be present at higher levels in SLE.4 Murine data suggest that an estrogen-mediated breakdown in B cell tolerance is genetically determined either by polymorphisms of the estrogen receptor genes or, more likely, by polymorphisms of estrogen-inducible genes or of other genes in pathways that involve estrogen-inducible genes.5
Benefits Beyond Birth Control
The clinical relevance of determining the safety of OCs in SLE extends beyond birth control. A well-established salutary effect of estrogen, clearly relevant to women with SLE, is the preventive effect on bone loss and increase in bone mass at the lumbar spine, radius, and hips. Estrogens suppress bone-resorbing cytokines such as interleukin-1 and interleukin-6 and exert positive changes in calcium homeostasis by restoration of a defective synthesis of 1,25–dihydroxyvitamin D and augmentation of intestinal calcium absorption. In a retrospective cohort of 702 women with lupus followed for 5,951 person-years, fractures occurred in 12.3% of the patients, a nearly five-fold increase compared to healthy women.6 In a separate study, osteoporosis was detected in 22.6% of 84 premenopausal SLE patients and appeared to be related to disease duration and use of glucocorticoids.7 Similar observations were noted in a combined (pre- and postmenopausal) cohort of 75 SLE patients, again emphasizing an association with the use of steroids.8 Although prospective studies of OCs have not been performed on glucocorticoid-treated premenopausal women, observational epidemiologic studies suggest that women who received OCs had higher adjusted bone mass density than women who did not.9