Also, autonomic neuropathy is frequently overlooked in patients with SjD, although the literature suggests that up to half [of patients] may have it. Autonomic symptoms, like dizziness, are often attributed to ‘just fibromyalgia’ though they have distinct treatments that can really help. To screen for autonomic neuropathy, I like to ask about unusual sweating patterns (e.g., ‘My head sweats a lot, but my body doesn’t sweat at all’) in addition to asking questions that get at orthostasis (e.g., ‘Do you have difficulty standing in line at the grocery?’)
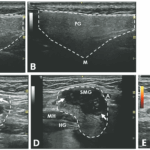
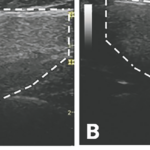
DD: I find salivary gland ultrasound really useful. A picture is worth a thousand words. In a patient whom you aren’t quite sure how active their glands are (e.g., Is there lymphoma in there or not?), I use imaging to be more objective. The ultrasound grading systems are really easy to understand, and you can follow imaging findings over time that could give you a reason to treat with something like rituximab if necessary.
If you don’t have access to a rheumatologist who is trained in musculoskeletal ultrasound, that’s okay. Just call your local radiologist, and ask for a head and neck ultrasound that focuses on the glands. Ask them to describe the glands and surrounding lymph nodes.
Conclusion
We will all take something different away from the wisdom shared by these SjD experts. Personally, I’ve already started recommending objective dryness testing more often for patients I would’ve previously diagnosed as just having fibromyalgia. It’s interviews and advice like this that really move the needle for me and my patients clinically, and I’m grateful for the opportunity that rheumatology affords me to keep learning.
 Samantha C. Shapiro, MD, is a clinician educator who is passionate about the care and education of rheumatology patients. She writes for both medical and lay audiences and practices telerheumatology.
Samantha C. Shapiro, MD, is a clinician educator who is passionate about the care and education of rheumatology patients. She writes for both medical and lay audiences and practices telerheumatology.
References
- Baer AN, Hammitt KM. Sjögren’s disease, not syndrome. Arthritis Rheumatol. 2021 Jul;73(7):1347–1348.
- Bernstein S. New video shows how to perform a lip biopsy to diagnose Sjögren’s syndrome. The Rheumatologist. 2021 Nov;15(11). https://www.the-rheumatologist.org/article/new-video-shows-how-to-perform-a-lip-biopsy-to-diagnose-sjogrens-syndrome.
- Lee AS, Scofield RH, Hammitt KM, et al. Consensus guidelines for evaluation and management of pulmonary disease in Sjögren’s. Chest. 2021 Feb;159(2):683–698. https://journal.chestnet.org/article/S0012-3692(20)34902-3/fulltext.
- Berardicurti O, Marino A, Genovali I, et al. Interstitial lung disease and pulmonary damage in primary Sjögren’s syndrome: A systematic review and meta-analysis. J Clin Med. 2023 Mar 29;12(7):2586. https://pmc.ncbi.nlm.nih.gov/articles/PMC10095380.
- Shiboski CH, Shiboski SC, Seror R, et al.; International Sjögren’s Syndrome Criteria Working Group. 2016 American College of Rheumatology/European League Against Rheumatism Classification Criteria for Primary Sjögren’s Syndrome: A consensus and data-driven methodology involving three international patient cohorts. Arthritis Rheumatol. 2017 Jan;69(1):35–45. https://pmc.ncbi.nlm.nih.gov/articles/PMC5650478.
- Zero DT, Brennan MT, Daniels TE, et al.; Sjögren’s Syndrome Foundation Clinical Practice Guidelines Committee. Clinical practice guidelines for oral management of Sjögren disease: Dental caries prevention. J Am Dent Assoc. 2016 Apr;147(4):295–305. https://pubmed.ncbi.nlm.nih.gov/26762707.