- Professional service — CPT defines “professional service” as “those face-to-face services rendered by a physician and reported by a specific CPT code(s)”; and
- Group practice — Single-specialty or multiple-specialty practices are considered a single “group” if they have the same tax identification number.
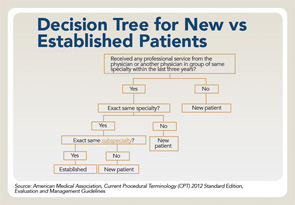
click for large version
Source: American Medical Association, Current Procedural Terminology (CPT) 2012 Standard Edition, Evaluation and Management Guidelines
Checklist to Determine Appeal Approach
- Verify the provider taxonomy codes — Healthcare Provider Taxonomy Codes are designed to categorize type, classification and/or specialization of healthcare providers. The code set consists of two sections: individuals and groups of individuals and non-individuals. They are updated twice a year, effective April 1 and Oct. 1. When applying for a National Provider Identifier (NPI) from the National Plan and Provider Enumeration System (NPPES), a healthcare provider must select the Healthcare Provider Taxonomy Code or code description that the healthcare provider determines most closely describes the healthcare provider’s type/classification/specialization, and report that code or code description in the NPI application. In some situations, a healthcare provider may potentially report more than one Healthcare Provider Taxonomy Code or code description in order to adequately describe the type/classification/specialization. Therefore, a healthcare provider may select more than one Healthcare Provider Taxonomy Code or code description when applying for an NPI, but must indicate one of them as the primary;
- Audit — It’s important to perform your own review or self-audit of the encounter to ensure the level of service billed is accurate. It’s important for practices to push back on the payer when claims are coded and documented appropriately;
- Use citations — Cite the Health Insurance Portability & Accountability Act (HIPAA) of 1996, specifically Administrative Simplification rules requiring providers and payers to use the HIPAA-approved datasets and guidelines. When appealing any claims that are down coded, quote the new and established definitions from the CPT book;
- Use an attachment to argue your point — The space provided on the appeal forms is inadequate to fully explain your point. Use this space to state “see attached explanation.” On the attachment, be sure to indicate the patient in reference to the claim, all identifying information related to the denial, the stated reason for the denial made by the carrier and your request to review the evidence included for a reversal of the denial; and
- Repeated problems with the same carrier or payer — The government has provided an Enforcement Tool—inform the payer that continued inappropriate denial or down coding of your claims due to lack of recognizing the taxonomy codes and definition of new vs. established patient is a violation under the new HIPAA Administrative Simplification and warrants you to report their noncompliance.
Knowing when to choose a “new” or “established” patient CPT code is important for compliance reasons as well as to maximize reimbursement. Additionally, it remains still vital for rheumatology practices to know the guidelines to bill the appropriate level of an E/M service (see the decision tree).

