
Evaluation and management (E/M) documentation and coding are not always clear. The E/M codes, a small group of CPT codes written by the American Medical Association (AMA), are the main billing codes for rheumatology practices. More and more practices are seeing denials because the patient is not determined by private payers and Medicare to be “new.” Services are frequently denied or coded down, requiring appeal. (Note: The CPT services referenced in this article are for educational use only. Copyright is held by the AMA.)
Background
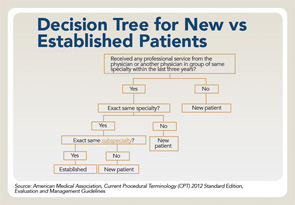
Prior to 2012, the definition was much broader and stated, “A new patient is one who has not received any professional services from the physician or another physician of the same specialty who belongs to the same group practice, within the past three years. An established patient is one who has received professional services from the physician or another physician of the same specialty who belongs to the same group practice, within the past three years.” To date, many insurance carriers as well as many Medicare Administrative Contractors are still using this definition. The new definition and how this might impact push back when E/M claims are inappropriately denied or coded down.
Current Definition
The new and established patient definitions in the E/M guidelines were further revised for CPT 2012, 2013 and 2014, and are present in the 2015 CPT to include important terms such as “exact” and “subspecialty,” as well as “qualified health care professional.” Please reference “New and Established Patient” under the Evaluation and Management (E/M) Service Guidelines in the front of your CPT book.
Based on the revisions made since 2011, subspecialties are now recognized for the determination of established vs. new patients. The revisions further clarify that although the physician or qualified healthcare professional may be of the same specialty, differences among subspecialties might require a new patient workup, rendering a new patient service rather than an established patient service. The following examples provide further clarification for the reporting of these services:
- New patient — A new patient is now defined as one who has not received any professional services from the physician/qualified healthcare professional or another physician/qualified healthcare professional of the exact same specialty and subspecialty who belongs to the same group practice, within the past three years; and
- Established patient — An established patient is now defined as one who has received professional services from the physician/qualified healthcare professional or another physician/qualified healthcare professional of the exact same specialty and subspecialty who belongs to the same group practice, within the past three years.
In order to determine if your patient is “new” or “established,” you will need to understand two terms used in CPT’s definition of a new or established patient: professional service and group practice:
- Professional service — CPT defines “professional service” as “those face-to-face services rendered by a physician and reported by a specific CPT code(s)”; and
- Group practice — Single-specialty or multiple-specialty practices are considered a single “group” if they have the same tax identification number.
Checklist to Determine Appeal Approach
- Verify the provider taxonomy codes — Healthcare Provider Taxonomy Codes are designed to categorize type, classification and/or specialization of healthcare providers. The code set consists of two sections: individuals and groups of individuals and non-individuals. They are updated twice a year, effective April 1 and Oct. 1. When applying for a National Provider Identifier (NPI) from the National Plan and Provider Enumeration System (NPPES), a healthcare provider must select the Healthcare Provider Taxonomy Code or code description that the healthcare provider determines most closely describes the healthcare provider’s type/classification/specialization, and report that code or code description in the NPI application. In some situations, a healthcare provider may potentially report more than one Healthcare Provider Taxonomy Code or code description in order to adequately describe the type/classification/specialization. Therefore, a healthcare provider may select more than one Healthcare Provider Taxonomy Code or code description when applying for an NPI, but must indicate one of them as the primary;
- Audit — It’s important to perform your own review or self-audit of the encounter to ensure the level of service billed is accurate. It’s important for practices to push back on the payer when claims are coded and documented appropriately;
- Use citations — Cite the Health Insurance Portability & Accountability Act (HIPAA) of 1996, specifically Administrative Simplification rules requiring providers and payers to use the HIPAA-approved datasets and guidelines. When appealing any claims that are down coded, quote the new and established definitions from the CPT book;
- Use an attachment to argue your point — The space provided on the appeal forms is inadequate to fully explain your point. Use this space to state “see attached explanation.” On the attachment, be sure to indicate the patient in reference to the claim, all identifying information related to the denial, the stated reason for the denial made by the carrier and your request to review the evidence included for a reversal of the denial; and
- Repeated problems with the same carrier or payer — The government has provided an Enforcement Tool—inform the payer that continued inappropriate denial or down coding of your claims due to lack of recognizing the taxonomy codes and definition of new vs. established patient is a violation under the new HIPAA Administrative Simplification and warrants you to report their noncompliance.
Knowing when to choose a “new” or “established” patient CPT code is important for compliance reasons as well as to maximize reimbursement. Additionally, it remains still vital for rheumatology practices to know the guidelines to bill the appropriate level of an E/M service (see the decision tree).
For more information on coding and billing E/M services appropriately, contact Melesia Tillman at [email protected] or 404-633-3777 x820.

