The higher the titer, the greater the likelihood that the patient has a rheumatic disease. There are, however, frequent exceptions to this rule, particularly among patients with one of the chronic inflammatory disorders noted above. Furthermore, the use of a higher titer for diagnosis decreases the sensitivity of the test at the same time as it increases the specificity. RF-positive patients with RA may experience more aggressive and erosive joint disease and extra-articular manifestations than those who are RF negative. Similar findings have been observed in juvenile RA. These general observations, however, are of limited utility in an individual patient because of wide interpatient variability. In this setting, accurate prediction of the disease course is not possible from the RF alone. RF titer rarely correlates with the degree of clinical activity.
Antibodies to Citrullinated Proteins
There has been considerable interest in developing a better test for the diagnosis of RA, which has greater sensitivity and specificity than the tests that detect RFs. Within the last decade, as an outgrowth of determining the molecular specificity of antifilaggrin, antikeratin, and antiperinuclear antibodies, it was recognized that many patients with RA have antibodies to citrullinated proteins. Proteins that are citrullinated have had an arginine replaced by citrulline, a minor amino acid. This posttranslational modification is mediated by the enzyme peptidyl arginine deiminase 4 (PAD4).
PAD4 is the form of PAD associated with RA. It has been found in bloodstream granulocytes and is localized in the cell nucleus. Its only known activator is a component in cigarette smoke, but its activation is also associated with inflammation. Much more work needs to be done to determine what specifically in RA activates (and downregulates) PAD. Because increased activity of PAD4 has been demonstrated in synovial fluid and synovium of patients with RA and other inflammatory arthritides, but generally not OA, it appears to be associated with inflammation. Citrullination of proteins has also been in noted in multiple sclerosis. The primary physiologic role for PAD enzymes (and the conversion of arginine to citrulline) appears to be related to regulation of nucleosome, that is, histone function. However, the development of antibodies to citrullinated proteins is relatively specific to RA.
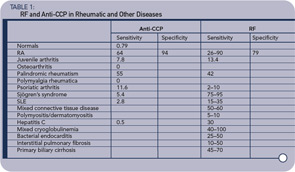
To facilitate analysis of antibodies to citrullinated proteins, a number of peptide antigens containing citrulline were created, although these have had a variable degree of sensitivity for recognizing patients with RA. However, a cyclic peptide containing citrulline was found to have a high sensitivity and was subsequently utilized to develop a commercial assay. This test, named anti-CCP (for cyclic-citrullinated peptide) has now been studied extensively, especially in Europe, and it has better sensitivity and specificity for the diagnosis of RA than tests that detect RF. A number of commercial firms have developed different assays for the detection of these antibodies to CCP, and the assays have been called CCP1, CCP2, CCP3, etc.