Next, the researchers used the model to calculate risk probabilities they thought corresponded with varying diagnostic certainty levels: unlikely, possible, likely and definite SLE. They used the validation cohort to assess the proportion of actual patients with SLE and control patients captured within each predicted SLE risk group. They found the calculated SLE risk probabilities correlated positively with disease severity and organ damage.
The investigators then used the discovery cohort to identify a cut-off to separate SLE from other rheumatic diseases. They chose the 50% risk probability threshold and found that at this threshold, the SLERPI demonstrated both high sensitivity (95.1%) and specificity (93.7%). SLERPI was accurate to 94.8% in the total validation cohort. When the team tested the cut-off against the control subset with undifferentiated connective tissue disease, the model specificity was 91.1%. The model also yielded very high rates of correct predictions within multiple SLE patient subgroups: for early SLE, a sensitivity of 93.8%; for lupus nephritis, a sensitivity of 97.9%; for neuropsychiatric lupus, a sensitivity of 91.8%; for hematological lupus, a sensitivity of 98.6%; for severe SLE, a sensitivity of 96.4%.
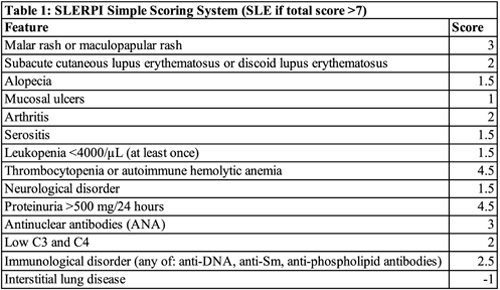
Finally, to facilitate the use of SLERPI in daily practice, the researchers converted their model to a simple scoring system. They found an operational cut-off score of 7 converted the logistic regression model into a simple scale for both clinical and serologic features of SLE (Table 1).
“Although I do not think machines can replace human/clinician assessment, I think this scoring system certainly has a role,” says Brett Smith, DO, a rheumatologist at Blount Memorial Physicians Group in Alcoa, Tenn. “If this were made available to primary care practices as a way to triage referrals to rheumatologists, it would provide a potentially reliable way to schedule referrals based on acuity or disease activity.”
Daniel J. Wallace, MD, associate director of the rheumatology fellowship program at the David Geffen School of Medicine Center, University of California, Los Angeles, disagrees. “This is an interesting study, but it really applies only to Greece,” he says. “We have a different health system, electronic medical records, and a different diversity of patients and cultures. Most of us diagnose lupus using our intuition, training and experience and don’t rely on algorithms.” He adds that not all predisposition factors for SLE will apply for all patients and he is concerned that an algorithm may lead to an inaccurate diagnosis and unnecessary treatment.