Additional workup with magnetic resonance imaging (MRI) of her brain revealed multiple, scattered, hyperintense foci throughout the deep white matter of the bilateral cerebral hemispheres of non-specific origin without an active demyelinating process. A magnetic resonance angiogram of her brain was negative for stenosis or occlusion. Cervical, thoracic and lumbar spine MRI revealed mild spondylosis without evidence of abnormal cord signal or enhancement.
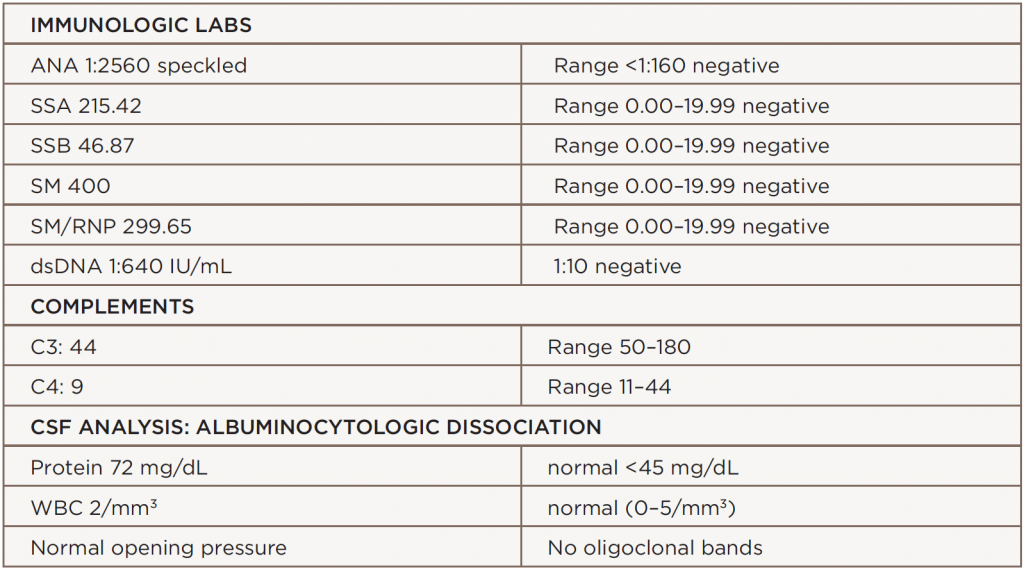
The patient was pulsed initially with high-dose methylprednisolone for presumed active SLE. After the CSF revealed an albuminocytologic dissociation, we made a diagnosis of Guillain-Barré syndrome. The clinical picture of ophthalmoplegia, ataxia and areflexia clinched further diagnosis of MFS variant of GBS.
Based on these findings, we initiated plasma exchange for five days. Steroids were gradually tapered over three days, and she was eventually continued on a low, maintenance dose. She remained stable and did not develop GBS progression, such as respiratory failure. Her diplopia, lateral gaze palsy and ptosis resolved over the course of one week. Her muscle strength measured 5/5 in all extremities. Her gait was normal at the time of discharge.
Discussion
SLE is an inflammatory disease without an identified cause that can target every organ system. Its protean features allow for dramatic disease variation among patients. It is characterized by immunologic abnormalities that affect women of child-bearing age.
Patients with SLE may develop a wide array of neurologic features. GBS has appeared in a small number of SLE case reports. Patients with its acute form typically present with an ascending areflexic motor weakness without sensory loss. Others can present with a combination of sensory and/or motor findings (see Table 1). The MFS variant classically presents with the triad of ophthalmoplegia, ataxia and areflexia.
MFS is a rare GBS variant with ocular involvement. This subset is estimated to encompass 5–10% of GBS cases, with an incidence of one in 1 million. One-quarter of patients with MFS will develop extremity weakness in some form, which is the connecting factor to GBS. There may be incomplete presentations of MFS that present with different combinations, such as acute ophthalmoplegia without ataxia, or acute ataxic neuropathy without ophthalmoplegia. In addition, it is possible to see bulbar and facial weakness as presenting symptoms. Ophthalmoplegia in MFS is possibly the result of highly dense concentrations of GQ1b gangliosides, which are found in abducens, trochlear and oculomotor nerves. This imbalance of ganglioside antigenic targets results in anti-GQ1b antibodies binding to these ocular nerves causing damage leading to aberrant muscle function.6 anti-GQ1b antibodies appear in 85–90% of patients with MFS and may be a confirmatory finding.