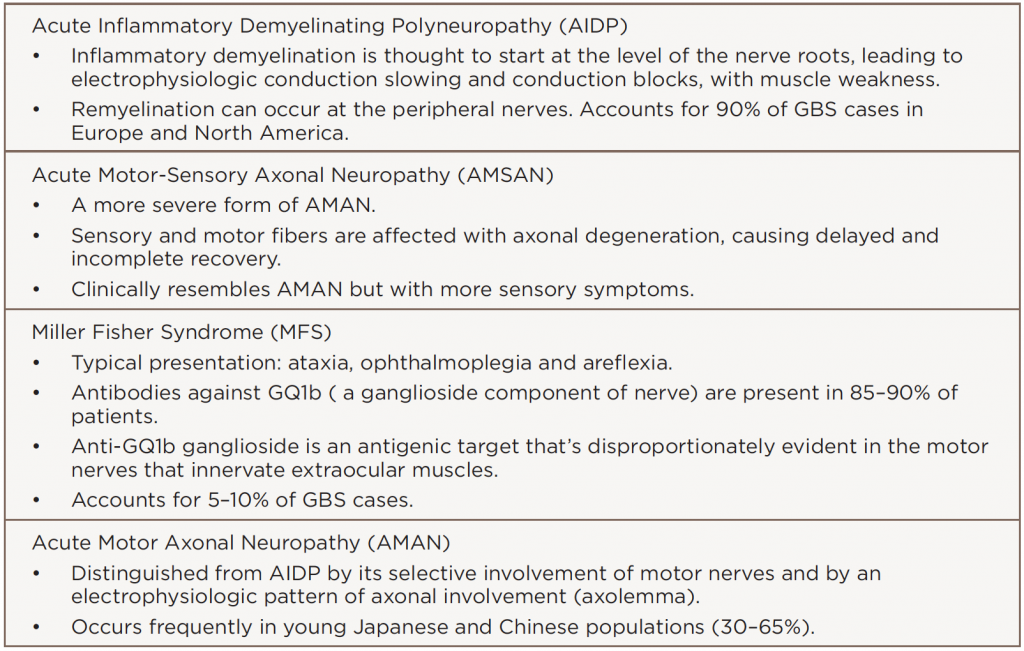
GBS has many variants (see Table 2). Although rare, Miller Fisher syndrome typically presents with ophthalmoplegia, ataxia and areflexia. GBS may also present as new- and acute-onset SLE.
Prompt recognition of MFS (as well as other GBS variants) is urgent given treatment challenges. Overall, the prognosis is good with early diagnosis of SLE and GBS. No set standard for treatment exists, so therapies are usually guided by disease severity.
Our patient responded well, with complete resolution of her neurological symptoms following plasma exchange and steroid administration. This patient had discoid lupus, positive anti-dsDNA and low complements, but after her GBS resolved, she developed proteinuria of 8 grams and underwent a renal biopsy. Her biopsy confirmed membranous glomerulonephritis, which was treated with mycophenolate mofetil 1,500 mg twice daily, along with prednisone and hydroxychloroquine 200 mg twice daily. She responded to this therapy with a decrease in proteinuria.
Bottom line: Be very diligent in SLE patients when they have persistently positive serologies. Our patient had MFS as unusual neurologic and renal complications of SLE. Both were successfully treated, and she is doing well at present.
Sedrick Bradley, MD, is a rheumatology fellow at Ochsner Medical Center, New Orleans. He completed his residency at the University of Mississippi Medical Center, Jackson, Miss. His clinical and research interests include systemic lupus erythematosus and the role of T cell homeostasis in rheumatoid arthritis.
Nirupa J. Patel, MD, is a clinical associate professor of medicine in the Section of Rheumatology at LSU Health Sciences Center, New Orleans. Her special interests include HIV infection and myositis.
References
- Willison HJ, Jacobs BC, van Doorn PA, et al. Guillain-Barré syndrome. Lancet. 2016 Aug 13;10045(388):717–727.
- Hughes RA, Wijdicks, EF, Barohn R, et al. Practice parameter: Immunotherapy for GBS. Neurology. 2003 Sep 23;61(6):736–740.
- Patwa HS, Chaudhry V, Katzberg H, et al. Evidence-based guideline: Intravenous immunoglobulin in the treatment of neuromuscular disorders: Report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2012 Mar 27; 78(13):1009–1015.
- Hughes RA, Swan AV, van Doorn PA. Intravenous immunoglobulin for Guillain- Barré syndrome. Cochrane Database Syst Rev. 2012 Jul 11;(7):CD002063.
- Raphael JC, Chevret S, Hughes RA, et al. Plasma exchange for Guillain-Barré syndrome. Cochrane Database Syst Rev. 2012 Jul 11;(7):CD001798.
- Chiba A, Kusunoki S, Obata H, et al. Serum anti-GQ1b IgG antibody is associated with ophthalmoplegia in Miller Fisher syndrome and Guillain-Barré syndrome: Clinical and immunohistochemical studies. Neurology. 1993 Oct;43(10):1911–1917.