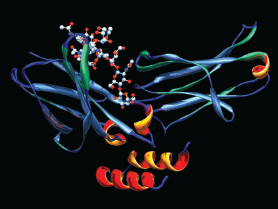
A computer model showing the secondary structure of the drug rituximab. The primary structure of an oligosaccharide (sugar), needed for the biologic activity of proteins, is at the upper left.
Dr. Mark J. Winter / Science Source
Patients with a diagnosis of rheumatoid arthritis (RA) experience on average double the risk of developing malignant lymphoma when compared with the general population. With the major changes in RA treatment taking place over the past decade, has there been a reduction in the risk of lymphoma in this population? Researchers from the Karolinska Institute in Stockholm Sweden set out to answer that question.1
“Given the dramatic changes in RA treatment brought about by the addition of biologic agents over the past 15 years, one could expect the lymphoma risk in contemporary patients to have decreased,” says Karin Hellgren, MD, PhD, from the Rheumatology Unit at Karolinska University Hospital. “However, in a previous report from our group, we still observed a doubling of lymphoma risk.”2
Extending Previous Assessment
They extended their previous assessment in a more recent cohort of RA patients, first diagnosed between 1997 and 2012. The group also looked for potential factors, such as RA characteristics and therapy, that may provide insight into predicting those who are at higher risk of being diagnosed with lymphoma at an early stage of the RA disease course.
“To do this, we took advantage of the unique possibilities offered by the Swedish health, quality and populations registers,” says Dr. Hellgren. “This enables links across different registries through the individual’s national registration number (NRN), which is assigned to all Swedish residents.”
Swedish Registries Gave Unique Information Possibilities

Dr. Hellgren
From the Swedish Rheumatology Quality (SRQ) register, the researchers assembled a cohort of 12,656 incident RA patients diagnosed between 1997 and 2012 with symptom duration less than 12 months between first RA symptom and diagnosis. They then obtained information on RA characteristics at baseline and at subsequent visits, including disease activity during the first year of follow-up.
The SRQ also allowed them to retrieve information on RA treatment with disease-modifying anti-rheumatic drugs (DMARDs) and oral corticosteroids during the first year of follow-up, and treatment with a tumor necrosis factor-alpha inhibitor (TNFi) at any time during follow-up.
From the Swedish population register, they randomly selected 10 population comparator subjects for each RA patient. Through linkage of the entire study population to the Swedish Cancer Register (coverage >95%), the researchers identified all registered cases of lymphoma, including date of diagnosis and subtype of lymphoma.
Results Show 60% Hazard Ratio Increase for Lymphomas
Sixty-two lymphoma cases were found during 79,239 person-years of follow-up. This corresponded to a crude incidence of 78 per 100,000 person-years. In the comparator cohort, 380 lymphomas occurred during 776,578 person-years or a crude incidence of 49 per 100,000 person-years.
Overall, the hazard ratio (HR) for lymphoma was increased in RA to 1.6 (95% confidence interval [95% CI] 1.2–2.1). Taking duration of disease into account, risk did not appear to decline over successive calendar years past initial diagnosis.
TNFi No Risk Impact Oral Corticosteroids Cut Risk in First Year
When medication usage was assessed, neither the use of methotrexate during the first year of diagnosis nor the use of TNFis ever increased lymphoma risk (HR 0.9 [95% CI 0.4–1.9]). Use of oral corticosteroids in the first year was associated with a reduced risk of lymphoma (HR 0.5 [95% CI 0.3–0.9]).
“There has been a longstanding concern that TNFi agents may induce lymphoma development,” says Dr. Hellgren. “In the present study, we found that there was no increased risk of lymphoma associated with TNFi therapy during the study period. There was also a lack of association between lymphoma risk and methotrexate treatment during the first year following RA diagnosis.”
Inflammatory Activity Not Predictive
Inflammatory activity during the first year after diagnosis was not predictive of future lymphoma risk. They found no association between risk and the 28-joint Disease Activity Score (DAS28) levels at diagnosis or one year of follow-up. Using DAS28 to estimate risk with respect to accumulated inflammatory activity during the first year was not significantly associated with either high or low aggregated values.
When the researchers looked at specific subtypes of lymphomas, chronic lymphocytic leukemia was seen less often than in the general population. On the other hand, Hodgkin’s lymphoma occurred more frequently.
“We concluded that the risk of lymphoma remains increased in a similar magnitude as was reported in historical cohorts,” says Dr. Hellgren. “Reassuringly, our standard early RA therapy during the first year following RA diagnosis and TNFi exposure any time during the study period does not seem to be associated with increased lymphoma risk in incident RA patients. On the contrary, we observed a reduced risk associated with oral corticosteroid use during the first year.”
She points out that the finding of inflammatory activity at diagnosis and in the first year following RA diagnosis was not a predictor of developing a future lymphoma. It is important to stress that this does not rule out that an accumulation of continuous inflammatory activity over many years could be important.
“From a lymphoma perspective, the finding of reduced risk in association with oral corticosteroids is of particular interest to clinicians given their anti-inflammatory effect profile,” says Dr. Hellgren.
This study confirmed that despite changes in modern therapeutic approaches to the treatment of RA, risk for developing lymphomas remains at the same levels seen in historical cohorts. However, although clinicians need to remain aware of the possibility of lymphoma development in RA patients, the absolute risks remains low.
Results Answer Patient Questions
The results should also inform physicians that early standard treatments are not associated with increased risk of lymphoma. Dr. Hellgren stresses that this is an important piece of information to give patients because it addresses some of their questions about the potential for harm from taking immune-modulating therapies over long periods of time.
The group’s findings are also interesting from an etiological standpoint. Although it could be expected that improved therapies may reduce the risk of lymphomas, this is not the case.
“One reason for this could be that we just haven’t been able to follow this group long enough to detect a reduction,” Dr. Hellgren says. “Another hypothesis that can’t be excluded is that the remaining increase in lymphoma risk indicates a shift from disease-related to treatment-related risk, although this, of course, remains speculative. Our results highlight the importance of continually evaluating lymphoma risk in association with not only TNFi agents, but also other agents including new upcoming ones.”
Kurt Ullman has been a freelance writer for more than 30 years and a contributing writer to The Rheumatologist for 10 years.
References
- Hellgren K, Baecklund E, Backlin C, et al. Rheumatoid arthritis and risk of malignant lymphoma: Is the risk still increased? Arthritis Rheumatol. 2017 Apr;69(4):700–708.
- Hellgren K, Smedby KE, Feltelius N, et al. Do rheumatoid arthritis and lymphoma share risk factors? A comparison of lymphoma and cancer risks before and after diagnosis of rheumatoid arthritis. Arthritis Rheum. 2010 May;62(5):1252–1258.