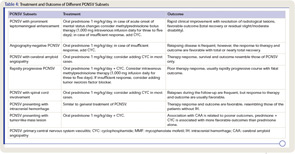
There is emerging evidence that therapy of PCNSV can differ among patients and that a uniform approach is not indicated (see Table 4). Relapses or recurrences were recorded in only 26% of the Mayo Clinic series.1 Patients with relapsing disease required longer therapy but otherwise had outcomes similar to those without relapses.
Therapy appears to be associated with a favorable outcome in most patients. In the Mayo Clinic series, most patients who had low disability at the time of diagnosis continued to have low disability at last follow-up; in contrast, most of the 22 patients with severe disability at diagnosis had less disability at follow-up.1
Serial MRI and MRA (four to six weeks after the beginning of treatment, then every three to four months during the first year of treatment, or in case of new neurological deficit), as well as repeat careful neurological examinations are useful to monitor the disease course. In patients with stable imaging but worsening clinical symptoms, a repeat spinal fluid exam and repeat angiography may be indicated.
Our understanding of PCNSV and the delineation of its spectrum and subsets has advanced, but further study is needed to clarify methods of diagnosis and optimal management.
Acknowledgments
We thank Drs. John Huston III, Teresa J.H. Christianson, Kenneth T. Calamia, James F. Meschia, Caterina Giannini, and Dylan Miller for their collaboration in clinical studies on primary central nervous system vasculitis; Dr. Huston for providing angiographic and MRI documentation, and Drs. Giannini and Miller for providing histopathological documentation.
Dr. Salvarani is director of the Unit of Rheumatology at Arcispedale S. Maria Nuova in Reggio Emilia, Italy. Dr. Brown is chair of neurology at the Mayo Clinic in Rochester, Minn. Dr. Hunder is professor emeritus at the Mayo Clinic College of Medicine in Rochester, Minn.
References
- Salvarani C, Brown RD Jr, Calamia KT, et al. Primary central nervous system vasculitis: Analysis of 101 patients. Ann Neurol. 2007;62:442-451.
- Benseler SM, Silverman E, Aviv RI, et al. Primary central nervous system vasculitis in children. Arthritis Rheum. 2006;54:1291-1297.
- Salvarani C, Giannini C, Miller DV, Hunder G. Giant cell arteritis: Involvement of intracranial arteries. Arthritis Rheum. 2006; 55:985-989.
- Cravioto H, Feigin I. Noninfectious granulomatous angiitis with a predilection for the nervous system. Neurology. 1959;9:599-609.
- Calabrese LH, Mallek JA. Primary angiitis of the central nervous system. Report of 8 new cases, review of the literature, and proposal for diagnostic criteria. Medicine (Baltimore). 1988; 67:20-39.
- Moore PM. Diagnosis and management of isolated angiitis of the central nervous system. Neurology. 1989;39:167-173.
- Kadkhodayan Y, Alreshaid A, Moran CJ, Cross DT 3rd, Powers WJ, Derdeyn CP. Primary angiitis of the central nervous system at conventional angiography. Radiology. 2004;233:878-882.
- Salvarani C, Brown RD Jr, Calamia KT, et al. Angiography-negative primary central nervous system vasculitis: A syndrome involving small cerebral vessels. Medicine (Baltimore). 2008; 87:264-271.
- Duna GF, Calabrese LH. Limitations of invasive modalities in the diagnosis of primary angiitis of the central nervous system. J Rheumatol. 1995;22:662-667.
- Eleftheriou D, Cox T, Saunders D, Klein NJ, Brogan PA, Ganesan V. Investigation of childhood central nervous system vasculitis: Magnetic resonance angiography versus catheter cerebral angiography. Dev Med Child Neurol. 2010;52:863-867.
- Küker W, Gaertner S, Nagele T, et al. Vessel wall contrast enhancement: A diagnostic sign of cerebral vasculitis. Cerebrovasc Dis. 2008;26:23-29.
- Salvarani C, Brown RD Jr, Huston J 3rd, Hunder GG. Prominent perivascular enhancement in primary central nervous system vasculitis. Clin Exp Rheumatol. 2008;26(3 Suppl 49):S111.
- Swartz RH, Bhuta SS, Farb RI, et al. Intracranial arterial wall imaging using high-resolution 3-tesla contrast-enhanced MRI. Neurology. 2009;72:627-634.
- Miller DV, Salvarani C, Hunder GG, et al. Biopsy findings in primary angiitis of the central nervous system. Am J Surg Pathol. 2009;33:35-43.
- Salvarani C, Brown RD Jr, Calamia KT, et al. Primary CNS vasculitis with spinal cord involvement. Neurology. 2008;70:2394-2400.
- Salvarani C, Brown RD Jr, Calamia KT, et al. Primary central nervous system vasculitis with prominent leptomeningeal enhancement: A subset with a benign outcome. Arthritis Rheum. 2008; 58:595-603.
- Salvarani C, Brown RD Jr, Calamia KT, et al. Primary central nervous system vasculitis: Comparison of patients with and without cerebral amyloid angiopathy. Rheumatology (Oxford). 2008;47:1671-1677.
- Salvarani C, Brown RD Jr, Calamia KT, et al. Rapidly progressive primary central nervous system vasculitis. Rheumatology (Oxford). 2001;50:349-358.
- Molloy ES, Singhal AB, Calabrese LH. Tumour-like mass lesion: An under-recognised presentation of primary angiitis of the central nervous system. Ann Rheum Dis. 2008; 67:1732-1735.
- Salvarani C, Brown RD Jr, Calamia KT, et al. Primary central nervous system vasculitis presenting with intracranial hemorrhage. Arthritis Rheum. In press.
- Ducros A, Bousser MG. Reversible cerebral vasoconstriction syndrome. Pract Neurol. 2009;9:256-267.
- Cupps TR, Moore PM, Fauci AS. Isolated angiitis of the central nervous system. Prospective diagnostic and therapeutic experience. Am J Med. 1983;74:97-105.
- Salvarani C, Brown RD Jr, Calamia KT, et al. Efficacy of tumor necrosis factor alpha blockade in primary central nervous system vasculitis resistant to immunosuppressive treatment. Arthritis Rheum. 2008;59:291-296.
- Sen ES, Leone V, Abinun M, et al. Treatment of primary angiitis of the central nervous system in childhood with mycophenolate mofetil. Rheumatology (Oxford). 2010;49:806-811.
- Holle JU, Gross WL. Neurological involvement in Wegener’s granulomatosis. Curr Opin Rheumatol. 2011;23:7-11.