By late October, as the nor’easter storms swept along the New England coast where she lived, she would rely on her supply of topical NSAID crèmes, which she would replenish while overseas. Mme. D was a believer in the utility of topical NSAIDs years before their adoption in the U.S. She faithfully applied topical diclofenac over her sore knees before consuming her daily bottle of Vichy Célestins mineral water. She maintained that the crèmes worked best in combination with a tall glass of Vichy Célestins mineral water. It had to be Vichy—no generic substitution! After all, Mme. D explained how the original spa at Vichy was built by Julius Caesar, and over the centuries was frequented by many seeking its medicinal magic, including the emperor Napoleon. The Vichy water’s striking mineral taste reflects its passage through the extraordinarily rich soil of the region. It flows at a constant temperature of 17.3° C under the rock formation that once formed the Convent of Celestine. Cheers!
For those European patients who prefer a more physical approach to their treatment regimen, they can choose from a menu of thermal baths, thermal showers, steam baths, thermal gas inhalation, and whirlpool mud therapies. Looking back, this Euro-style regimen must have done Mme. D. some good. She lived a full life, and when she died at age 91, her medication list, save her crèmes, was still blank. She never required any surgical procedures to treat her severe knee osteoarthritis or, as they say in Europe, gonarthritis.
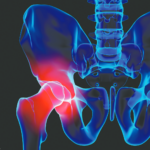
I often wondered whether the Swiss government was wasting taxpayer money covering her spa therapy, mineral water supply, and topical gels. Is there any objective evidence to support such a holistic approach for treating osteoarthritis, the bane of the aging skeleton? Can a patient’s subjective improvement from wallowing in sulfurous mud or relaxing in radon-enriched carbon dioxide baths be measured objectively?
In 2009, French rheumatologists working at Aix-les-Bains (where, 90 years earlier, Jacques Forestier plied his trade and described the benefits of gold therapy in RA) performed a meta-analysis of 19 randomized clinical trials of spa therapy based on the clinical guidelines of the French National Authority for Health and the European League Against Rheumatism (EULAR). They concluded that spa therapy (also known by its august appellation, balneotherapy) provided benefits that lasted for at least 12 weeks in treating chronic low back pain, stable RA, ankylosing spondylitis, fibromyalgia, and osteoarthritis of the knees and hands. A Cochrane meta-analysis of balneotherapy for the treatment of RA was less sanguine. This review found that most of the studies were methodologically flawed to some extent. However, one study observed a significant short-term benefit for pain reduction when comparing mineral baths to cyclosporine A. I can only imagine seeking a prior authorization from one of our friendly health insurers for the coverage of a patient’s spa therapy.
I have asked many of my RA patients who have successfully weaned off steroids what they thought about the concept of taking prednisone in addition to their methotrexate. To a person, they related how they never wanted to go back on steroids.
Don’t Spare the Steroids?
But now, some of our European colleagues are challenging one of the most basic tenets of clinical rheumatology; that is, whether or not corticosteroids should be considered to be a disease-modifying drug therapy for RA. A recent study from the Netherlands analyzed the effect of adding 10 mg of prednisone daily to a weekly regimen of methotrexate in patients with RA.4 The authors concluded that the addition of prednisone not only improved the patients’ functional status, but it also significantly reduced the degree of radiographic damage observed after two years. This paper, published in the Annals of Internal Medicine, follows a line of several similar smaller studies claiming a newfound status for using corticosteroids in patients with RA. An accompanying editorial opined that, “a very short period of high-dose [emphasis added] glucocorticoid therapy (for example, 60 mg of prednisone daily tapered to 7.5 mg daily over 6 weeks), when used as part of combination therapy, can control symptoms and radiographic disease progression to the same extent as anti–tumor necrosis factor therapy.”5 Is this heresy or innovation? What happened to the long-held notion of always searching for a “steroid-sparing agent” for our patients? After all, most clinicians try to minimize their patients’ steroid exposure in order to mitigate potential side effects.