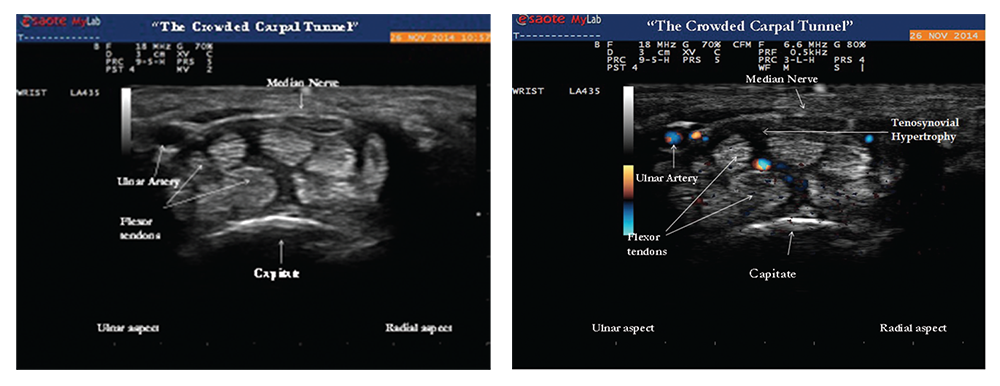
nocturnal hand paresthesias. His physical examination was significant for subtle soft tissue swelling over the left first metacarpophalangeal (MCP) joint with an impression of fullness over the volar aspect of the left wrist upon inspection (see Image 1). On palpation of the involved joints, he had minimal tenderness. Ultrasound of the volar wrist within the carpal tunnel revealed tenosynovial hypertrophy along with strikingly positive power Doppler signals on both longitudinal and transverse views consistent with active tenosynovitis (see Image 1, above).
The median nerve was normal in cross‑sectional area (9 mm2) and appeared hypoechoic, but was significantly enlarged compared with a more proximal portion of the median nerve (6 mm2). A size ratio comparison of distal to proximal median nerve (9 mm2/6 mm2) was calculated to be 1.5 and ratios greater than 1.4 are suggestive of median nerve entrapment.2 The ultrasound findings of carpal tunnel syndrome are also defined by enlargement of the median nerve by cross-sectional area of measurements equal to or greater than 12 mm2. In the clinical context of hand paresthesias, the ultrasound images of distal median nerve enlargement suggest carpal tunnel syndrome and this was confirmed by electromyographic nerve conduction studies (see Images 2 and 3).
(click for larger image)
Images 2 & 3: Gray-scale image (left) of the transverse view of the wrist showing tenosynovial hypertrophy within the proximal portion of the carpal tunnel. The hazy dark areas between the flexor tendons represent tenosynovial proliferation with effect of “crowding” the carpal tunnel by increasing perineural median nerve pressure. Doppler ultrasound (right) of the same area reveals positive power Doppler signals between the flexor tendons, an abnormal finding consistent with tenosynovitis.
The patient was nihilistic and reluctant to take medications because he was still able to function with his symptoms; however, ultrasound provided objective evidence that convinced him to start disease-modifying anti-rheumatic drug (DMARD) therapy. The patient agreed to start etanercept therapy and understood the importance of subsequent follow-up care for proper treatment of his rheumatic disease.
Per the 2010 rheumatoid arthritis classification criteria, joint involvement, serology, acute-phase reactants and duration of symptoms are used for the diagnosis of RA. Patients with typical patterns of joint involvement (>10 joints with at least one small joint) and duration of symptoms for more than six weeks meet the clinical criteria for RA.3 The exclusion of RA mimics, such as viral and crystalline arthropathies, is critical to an accurate diagnosis.