CHICAGO—In the basic science session, Beyond NETs: Alternative Roles of Neutrophils in Spondyloarthritis, neutrophils are explored as a common pathophysiologic thread among the spondyloarthropathies. In this two-part talk, Dennis McGonagle, PhD, professor of investigative rheumatology at the Leeds Institute of Rheumatic and Musculoskeletal Medicine at St James Hospital, Leeds, England, opens by examining the role of neutrophil-derived interleukin (IL) 23 in spondyloarthropathy spectrum disorders. To close, Nigil Haroon, MD, PhD, MBA, professor and division head in rheumatology at the University of Toronto, details a series of experiments unraveling the MIF-HIF (macrophage migration inhibitory factor; hypoxia-inducible factor) axis, how neutrophils may be implicated and its role in spondyloarthritis pathogenesis.
The Role of Neutrophil IL-23 in Spondyloarthropathy Spectrum Disorders
Dr. McGonagle’s presentation, based on his 2023 Lancet Rheumatology paper by the same name, explored the pathologic role of neutrophil-derived IL-23 in the spondyloarthropathies, including axial spondyloarthritis, psoriatic arthritis and inflammatory bowel disease.1 He began by reviewing basic neutrophil biology, emphasizing their ubiquity, short half-lives and role as the first line of defense against microorganisms.
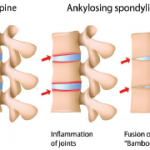
He highlighted the overlapping clinical features in the spondyloarthropathies and the numerous clinicopathologic findings that suggest a neutrophilic fingerprint, including Munro’s abscesses in the skin, crypt abscesses in the gut, neutrophilic inflammation in enthesitis, and hypopyon in anterior uveitis, as well as pyoderma gangrenosum and hidradenitis suppurativa. Driving this inflammation, he highlighted the IL-23/17 pathway, a T cell-neutrophil axis active in spondyloarthritis, in which neutrophil-derived IL-23 activates T cells, leading to production of IL-17A, IL-17F and tumor necrosis factor (TNF) alpha, with subsequent amplification of neutrophilic inflammation. In other words, rather than simply acting as foot soldiers, neutrophil derived IL-23 may be able to regulate T cell responses in some tissue compartments, which may help explain the lack of effectiveness of IL-23 inhibitors in ankylosing spondylitis.
Dr. McGonagle described the spondyloarthropathies as a “mixed pattern diseases”, meaning that they have MCH class I associations as well as autoinflammatory components – a sort of “hybrid state between pure innate and autoimmunity.”2 He introduced the term MHC-I-opathy, proposing that target tissues in spondyloarthritis exposed to environmental and mechanical stress trigger secondary adaptive immunity via CD8 positive T-cells, leading to IL-17 production and prominent neutrophilic inflammation.3
Considering the role neutrophils play in managing extracellular infections, it seems logical that they would mediate inflammation in the gut and skin, but what is their role at the enthesis?
He highlighted the work of Raimondo et al., demonstrating that IL-17 inhibition with sekukinumab leads to reduction of entheseal granulocytes.4 Likewise, in a mouse model for spondyloarthritis, the addition of IL-23 to IL-23 positive receptor cells led to upregulation of IL-17A and F, resulting in an abundance of myeloid cells and clinical enthesitis.5 Bridgewood et al. demonstrated that resident macrophages in the marrow of entheses make IL-23, and when examining the human enthesis at the spine, they found abundant inducible IL-23 production from neutrophils.6 In an SKG mouse model of spondyloarthritis, histological examination of the enthesitis demonstrated early appearance of MPO positive neutrophils and examination of gene expression identified numerous active neutrophil related genes and pathways.7