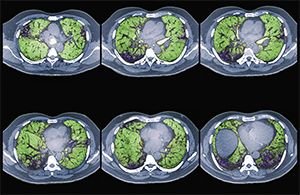
Colored CT scans of axial sections through the chest of a 68-year-old patient with ILD.
Zephyr/ScienceSource.com
CHICAGO—Interstitial lung disease (ILD) is challenging for the rheumatologist because there is little high-quality evidence to guide treatment decisions. A presentation at ACR Convergence 2025, The Many Faces of ILD, addressed some of these issues.
“Treating ILD feels a bit like a pick your own adventure,” said Erin Wilfong, MD, PhD, of Vanderbilt University Medical Center. “That’s because there are multiple options that, for a given patient with their particular disease, may be reasonable and the right choice.”
Articular Involvement Treatment
Dr. Wilfong first discussed rheumatoid arthritis with ILD (RA-ILD). Articular involvement is an important treatment variable because of an impact on mortality. A moderate to high clinical disease activity index is linked to changes in the survival curves with or without abnormal pulmonary function testing (PFT).1
There are many choices available. Methotrexate is not absolutely contraindicated in RA-ILD. A study by Dr. England, et. al found no differences in outcomes between tumor necrosis factor (TNF) inhibitors and non-TNF inhibitors in hospitalizations, mortality or respiratory mortality.2 Dr. Wilfong suggests there is no reason to avoid these therapies without contraindications or continuing progression.
What medications are useful if initial treatment proves ineffective? Azathioprine, mycophenolate (MMF) and rituximab have been shown to stabilize RA-ILD. This is true even for patients with a usual interstitial pneumonia (UIP) pattern.3
“If you treat the joints, you help the lungs,” said Dr. Wilfong. “There is no one right answer. The right answer is what works for your patient.”
SSc-ILD Treatment Data
Systemic sclerosis with ILD (SSc-ILD) differs from ILD in systemic autoimmune rheumatic diseases (SARDs) because there are high-quality data informing treatment decisions. In the Scleroderma Lung Study II, both MMF and oral cyclophosphamide worked, with the former being better tolerated. This study enrolled all comers, making it applicable to all SSc-ILD patients.4
Other options include tocilizumab, rituximab and nintedanib. All may be combined with MMF, and a subgroup analysis from the SENSCI trial indicates MMF and nintedanib may work synergistically.5
Manage Anti-Synthetase Syndrome Quickly
If you suspect anti-synthetase syndrome, quick treatment is important. Even with a UIP pattern, patients still benefit from immunosuppression. If treated with immunosuppression, progression-free survival improves and medial transplant-free survival increases 10-fold.6
“Remember that a transplant only lasts for five to seven years,” said Dr. Wilfong. “We need to treat people early to buy time before starting their transplant clock.”
