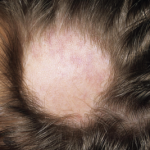
The first signs of alopecia areata (AA) often occur when the patient is in his or her 20s. Young adults afflicted with AA lose their hair, but their hair follicles remain intact, unscarred by the disease process. The disease process is puzzling.
Previous studies have demonstrated that the symptoms of AA occur when T cells attack the hair follicles. The concept of AA as an autoimmune disease is reinforced by the fact that patients with AA have higher rates of other autoimmune diseases than the general population.
Genome-wide association studies (GWAS) of AA have suggested that patients with AA are also predisposed to have certain polymorphisms of ligands for the natural, killer cell-activating receptor NKG2D. In particular, products of the KLRK1 gene have been implicated in disease pathogenesis. GWAS have also implicated the ɣC cytokine-receptor pathway, including interferon ɣ (IFNɣ) in the pathogenesis of AA.
The understanding that both the ɣC cytokine-receptor pathway and IFNɣ are involved in AA suggests that there may also be a role in pathogenesis for downstream signaling via Janus kinase (JAK) molecules. Unfortunately, up until now, the immune pathways in AA have not been defined. Thus, it has been difficult for investigators to develop rational targeted therapies for patients with AA.
Luzhou Xing, PhD, an assistant professor at Seton Hall University in South Orange, N.J., and colleagues published their analysis of the immune pathways required for autoreactive T cell activation in AA in the September issue of Nature Medicine.1
In an accompanying editorial, Sherrie J. Divito, MD, PhD, and Thomas S. Kupper, MD, both dermatologists at Harvard Medical School in Boston, describe the research as an “elegant synergy of genetic data from GWAS, of human and mouse data, and new in vivo and in vitro studies dissecting the mechanism of disease.”2
Xing et al begin their paper by reporting that cytotoxic CD8+NKG2D+ T cells can induce AA in a mouse model of the disease. Moreover, the investigators found that blocking IFNɣ, interleukin-2 or interleukin-15 receptor β with antibodies prevented development of the disease. The antibodies also reduced the accumulation of CD8+NKG2D+ T cells in the mice’s skin. When the researchers systematically administered pharmacological inhibitors of JAK family protein tyrosine kinases, they eliminated the IFN signature and prevented the development of AA in the mice.
“We next asked whether systemic tofacitinib treatment could reverse stablished disease by initiating therapy seven weeks after grafting, a point at which all mice had developed extensive AA,” Xing et al write. “Systemic therapy resulted in substantial hair regrowth all over the body, reduced the frequency of CD8+NKG2D+ T cells and reversed histological markers of disease, all of which persisted two–three weeks after the cessation of treatment.” Topical administration of protein tyrosine kinase inhibitors was also found to reverse established AA in mice.