“What can I eliminate from my diet to cure my arthritis?” is the question every client with arthritis asks me. Numerous case reports document patients who achieved lower markers of inflammation and reduced pain and stiffness associated with the removal of one or two food groups from a diet, but historically, no compelling evidence has indicated that what you eat could influence the course of the disease. Therefore, the usual answer has been, “You can eat whatever you want to eat.”
Fast forward to 2025, and you can now find an abundance of articles on nutrition and arthritis. Two main approaches to arthritis and nutrition exist: a whole diet approach vs. a specific foods approach. New avenues being explored include the influence of the gut microbiota and fasting.
Current Research
In the past decade, nutrition research has shifted to focus on a whole-diet approach to managing disease rather than looking for a single food or nutrient as the cause of disease. This is also true for arthritis. There is evidence that following a Mediterranean eating pattern leads to lower levels of disease activity and lower levels of pain and stiffness.1 Another study has shown an anti-inflammatory diet resembling the Mediterranean eating pattern also reduces disease activity.2
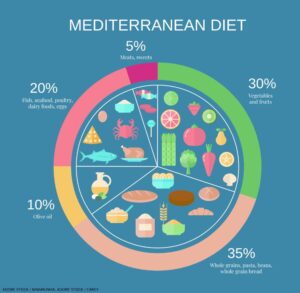
In general, a Mediterranean-style diet has fewer red meats and refined carbohydrates than a typical American diet. It emphasizes fruits and vegetables, whole grains, nuts and legumes, lean meats, fish and healthy fats.
The Mediterranean diet helps reduce disease activity, pain and stiffness by encouraging adequate consumption of various nutrients involved in various pathways that reduce inflammation. Those nutrients include omega-3 fatty acids, vitamin D, minerals and plant nutrients.3-5 At the same time, following the Mediterranean eating pattern leads to a reduction in the consumption of foods believed to increase inflammation and obesity (a separate driver of inflammation): ultra-processed foods, especially sugar, sweetened beverages, sweets and desserts, refined carbohydrates and meat.6,7
Vegan and vegetarian diets have also been studied, but the results are less consistent than a Mediterranean eating plan. This could, in part, be due to study design or to the difficulty some participants have in following these eating patterns because they are very different from the typical North American diet.
Many researchers focus on finding specific foods that cause arthritis. To date, the foods most often investigated are those that contain gluten and dairy products. Many case reports suggest these foods may be involved in development and management of arthritis. However, the evidence remains low grade.