Rheumatologists and many other physicians are deeply concerned about the decrease in Medicare reimbursement for dual energy X-ray absorptiometry (DXA) and vertebral fracture assessment (VFA) that took effect on January 1. The current reimbursement schedule will reduce practice expense reimbursement from the 2006 levels of approximately $140 for DXA and $40 for VFA to $40 and $25, respectively, by 2010—less than it costs to actually perform and interpret the tests.
“The proposed rates of reimbursement simply will not make up the expense of doing it in the physician’s office,” says Steven Petak, MD, president of the American Academy of Clinical Endocrinologists (AACE), and immediate past president of the International Society for Clinical Densitometry (ISCD). “If this goes into effect, my practice may have to stop seeing new Medicare patients. It’s a heartbreaking decision, but otherwise we’d go bankrupt.”
The cuts are due in part to a program of general governmental belt tightening mandated by bill S.1932, better known as the Deficit Reduction Act of 2005 (DRA). The DRA resulted from a congressional budget resolution to reduce spending by about $35 billion from 2006 to 2010. According to Congressional Budget Office estimates, enacting the DRA as written would reduce direct congressional spending by a total of $99 billion from 2006 through 2015. The net savings on Medicare and Medicaid combined over that time period would be $11.2 billion.
The bill requires reimbursement for imaging services to be cut by a total of $2.8 billion from 2007 to 2010, and by $8.1 billion through 2015. This would be accomplished, in part, by capping payment for the technical component of the exam—that is, the actual performance of the examination, rather than the interpretative aspect—at the rates paid for an exam performed in a hospital, even if it is actually performed in a physician’s office. Congress lumped DXA and VFA in with other imaging studies like PET and CT, even though the bone-density exams are simpler and less expensive to perform.
Additional reimbursement cuts to DXA happened through the Centers for Medicare & Medicaid’s (CMS’) five-year review process and when CMS changed the way it calculates practice expense.
Why a Reduction?
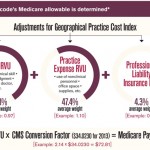
Every five years, the CMS must review the rates at which Medicare reimburses doctors for various treatments and procedures and, when necessary, adjusts them to reflect changes in technology, utilization, and other factors. The Medicare Physician Fee Schedule has three components: work, consisting of the actual physician work of performing a given treatment or test; practice, such as non-physician work time, equipment and supplies; and professional liability. In 2006, CMS also had to take into account the provisions of the DRA as it determined what changes, if any, to make in the work and practice portion of the fee schedule. To help guide their decisions, CMS officials rely on advice from the Relative Value Scale Update Committee (RUC) convened by the AMA. The RUC, in turn, makes recommendations based on its examination of any new data and the opinions of expert consultants.
When it came to determining reimbursement changes for DXA and VFA, the American College of Radiology shared with the RUC a survey of its members, who say that DXA scans took them an average of eight minutes to perform. They opined that the basis for calculating reimbursement for the work component should remain at its current level of 0.3 relative value units (RVUs), the scale used by CMS and most private insurers to determine physician reimbursement rates. Despite this recommendation, the RUC pegged reimbursement at 0.2 work RVUs, stating that it took physicians an average of only six minutes to perform a DXA. The ACR, along with other societies, sent a letter to Mark McClellan, MD, PhD, the CMS Administrator at the time, requesting that the RVUs remain at 0.3. CMS convened a refinement panel to allow the societies to present their case why the code should remain at 0.3. The ACR worked with ISCD to survey members across the United States to ascertain the actual work performed. The survey results indicated that the RVUs should remain at 0.3 or higher. This information was presented to the refinement panel. However, at the end of the refinement panel, a calculation of votes determined the final RVUs and the DXA RVU stayed at 0.2.
DXA also received a reimbursement cut from the practice expense portion of the Medicare calculation. CMS released a rule in 2006 changing the formula for practice expense. Previously, practice expense had been calculated using a top-down method; the new formula calculates direct practice expense in a bottom-up method. When the direct expenses for DXA were run through the new formula, reimbursement for the study was greatly reduced. Again, the ACR and several other societies told CMS that the calculation was unfairly reducing the reimbursement for DXA studies. In response, CMS reviewed the practice expense involved with DXA studies during its RUC meeting in San Diego earlier this month. The ACR, in conjunction with several other specialty groups, compiled practice expense information and presented its findings to the RUC at this meeting. At press time, CMS was still considering this additional information.
For its part, CMS has released a fact sheet noting that it has implemented substantial increases in payments for evaluation and management services such as office visits “so that physicians can spend more time with their patients to manage their care and achieve better outcomes.” The ACR surveyed the membership and worked with several other societies to assist in achieving the increase for E&M. And, “even after accounting for the payment decreases for DXA and CAD [computer-aided digital mammography], there would be hundreds of millions in additional spending directed to physicians to manage women’s healthcare, due to the increases for evaluation and management services.” What’s more, the CMS states that it is “revising coverage policy for bone-mass measurements to insure that women who need these tests to reduce the risk of osteoporosis can get them.”
The current Medicare reimbursement schedule will reduce practice expense reimbursement from the 2006 levels of $140 for DXA and $40 for VFA to $40 and $25, respectively, by 2010.
Possible Effects on Patient Care
CMS has yet to present any details on the promised policy revisions, however, and many observers believe that the current reimbursement schedule will have a profound impact on doctors’ ability to offer DXA and VFA to every appropriate candidate. “Our biggest concern is that it will limit access to care. The result will be that fewer people will be diagnosed with osteoporosis and fewer will be treated,” says Andrew Laster, MD, a rheumatologist and chair of the Public Policy Committee of the ISCD.
“Two-thirds of all DXA and VFA machines are in private offices, so physicians in private practice will be affected the most,” he adds.
“If these cuts go through, the work RVU for DXA will be equivalent to that for a finger X-ray,” says Sanford Baim, MD, a rheumatologist and associate clinical professor of medicine at the Medical College of Wisconsin in Milwaukee.
Interestingly, the reductions imposed by the CMS run counter to the recommendations that appeared in “Bone Health and Osteoporosis: A Report of the Surgeon General,” published in 2004. “Federal initiatives encourage people to get more DXA screening,” Dr. Laster points out. “It’s often included in the ‘Welcome to Medicare’ exam. There seems to be a disconnect between the people setting the policy and those who are enacting the RVUs.”
“These cuts make no pharmacoeconomic sense,” says Thomas Olenginski, MD, an associate in rheumatology at Geisinger Medical Center in Philadelphia. “They’re counter-intuitive, and they defeat the purpose of screening and intervention. The CMS does not appear to want to reward the work effort that goes into doing this.”
But the fight isn’t over yet. The ACR, along with the ISCD, the National Osteoporosis Foundation, and several other clinical and patient advocacy groups, is planning a two-part approach for 2007, says Joseph Flood, MD, chair of the ACR’s Government Affairs Committee. First is a public awareness campaign, to make sure people realize their access to DXA and VFA may be curtailed. The second is yet another appeal to the CMS, this time at a higher level.
If these measures fail and the cuts remain as proposed, some doctors may be forced to stop doing the studies altogether, warns Dr. Olenginski. “They’re going to have to make a business decision, and I can’t blame them for doing that.”
Norra MacReady is a medical journalist based in southern California.