Lightspring / shutterstock.com
Patients with polymyalgia rheumatica (PMR) or peripheral arthritis may require extra vigilance during treatment because of a suspected link to giant cell arteritis (GCA) and, potentially, permanent vision loss. “Development of giant cell arteritis after treating polymyalgia or peripheral arthritis: a retrospective case-control study,” a March 2018 study published in The Journal of Rheumatology, suggests rheumatologists should be on the lookout for cranial signs and symptoms in patients with PMR or peripheral arthritis because these can portend more serious outcomes related to the development of GCA.
Rationale
The frequency of late GCA following a diagnosis of PMR is controversial. This study examined the development of GCA in patients who were previously diagnosed with isolated PMR or peripheral arthritis. Lead author Eric Liozon, MD, Department of Internal Medicine, University Hospital of Limoges, France, and his colleagues sought to define risk factors for late GCA development after pure PMR diagnosis and the principal characteristics of the condition.
“As hospital-based internists involved in the clinical management of PMR and GCA patients, as well as in clinical research on GCA, Hubert de Boysson, MD, MSc, from Caen’s University Hospital [Caen, France], and I have repeatedly observed cases of true PMR evolving into GCA, even after years of follow-up,” Dr. Liozon says. “Two recent studies from Spanish researchers emphasized the ischemic visual risk of GCA occurring in patients with established PMR. However, [neither] of these studies was case controlled. Thus, we were interested in verifying these findings in a case-controlled study and [searching] for other relevant characteristics, both at the initial phase of PMR and at late-onset of vasculitis.”
Study Methods & Results
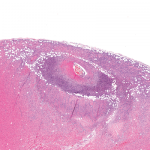
Researchers retrospectively compared clinical, laboratory and pathological characteristics of 67 patients at the onset of PMR or peripheral arthritis, and their treatments and outcomes, to those of a random group of 65 patients with PMR or peripheral arthritis who did not develop late GCA. Researchers included patients with prior peripheral arthritis (isolated or with PMR) because peripheral arthritis is frequently associated with PMR and may sometimes form part of the rheumatic spectrum of GCA. Researchers also compared the characteristics and outcomes of patients with late GCA with those of a random sample of patients with more usual GCA (65 with concurrent PMR or peripheral arthritis and 65 without). The entire cohort of 132 patients with PMR or peripheral arthritis (67 late GCA patients and 65 controls) was followed for an average of 38.5 months.
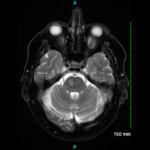
Patients with late GCA represented 7.4% of all GCA patients in the hospital-based inception cohort. GCA was diagnosed an average of 27 months after PMR or peripheral arthritis. Permanent visual loss developed in 10 patients, including eight of 48 (17%) who developed cranial arteritis. Patients with either form of GCA—usual or late—experienced similar outcomes.
At disease onset, patients with late GCA and controls were indistinguishable, except for a higher proportion of women in the late GCA group. The groups were similar in terms of baseline erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels, as well as proportions of patients experiencing long-lasting remission, relapses and resistant PMR or peripheral arthritis.
Cranial arteritis was the sole or prominent clinical feature in 48 patients (72%) and was typical (presenting with three or more of the following features: new-onset headache of moderate to severe intensity, jaw claudication or trismus, other jaw/mouth/throat problems, scalp tenderness, and an abnormal temporal artery on physical examination) in 33. Of these 48 patients, eight (17%) developed permanent visual loss (bilateral in three). Twelve patients exhibited transient, visual ischemic symptoms, and four of these developed permanent vision defects. In total, 18 patients (27%) developed visual ischemic symptoms, and all but one exhibited other features of cranial arteritis. Four other patients had extraocular permanent ischemic manifestations. Additionally, subclinical aortitis, headache, and fever were less often associated with late GCA than with the more usual form of GCA.
“Our study demonstrated that late GCA involves a visual ischemic risk that is similar to that of more usual forms of GCA and, therefore, not absorbed by a previous (or current) glucocorticoid treatment for a PMR,” says Dr. Liozon. “As in usual GCA, the risk of permanent visual loss in late GCA is increased in the presence of cranial signs and symptoms, albeit not always prominently, but is much lower in patients featuring systemic symptoms alone or associated with active PMR without cranial features. the implication of this is that any PMR patient (treated or recovered) who recalls persistent cranial symptoms should urgently be explored for a possible late GCA.”
Additional findings showed that of the 20 patients with negative temporal artery biopsy (TAB) (18) or no TAB (2), 12 had large vessel vasculitis evident in positron emission tomography (PET) or computed tomography (CT) scans. Of the 10 patients with previously negative TAB, eight had positive contralateral TAB data at the time of GCA diagnosis. Sixteen patients (24%) had prominent systemic disease mainly diagnosed by fluorodeoxyglucose (FDG)-PET; of these 16, only one (6%) experienced visual damage.
Implications
“Based on [these] results, patients with isolated PMR do not require more intensive medical care, as long as they do not develop atypical symptoms or signs,” Dr. Liozon says. “rather, our message to rheumatologists is to suggest that they keep in mind that every case of PMR [carries] a risk of developing GCA, notably (but not solely) during the first two years following diagnosis.”
Specifically, Dr. Liozon recommends physicians consider the following:
- Regularly ask these patients if they have cranial or ear, nose, and throat symptoms suggesting GCA;
- If they do, perform a careful examination of the temporal arteries, and perform a search for a bruit over axillary/humeral arteries. If any abnormalities are discovered, perform additional workups; and
- For any otherwise unexplained, persisting acute phase response in a patient with controlled or recovered PMR, order imaging of the patient’s aorta.
Dr. Liozon notes, “18F-FDG PET/CT is an effective imaging modality for detecting silent aortitis. Since [a] PET/CT scan often discloses the presence of large vessel vasculitis (LVV) in PMR patients, careful selection of those who really need it is crucial.”
Researchers also note that a “questionable female predominance was the only distinguishing feature of PMR or peripheral arthritis evolving into GCA,” but this should not necessarily affect practice.
“Although we found a strong association between female sex and the risk of late GCA, this finding may be inconsistent since the control cohort of PMR patients recruited in internal medicine was highly biased toward male patients,” Dr. Liozon says. “Accordingly, this should have no practical implication for clinicians who care for PMR patients.”
Dr. Liozon had the following advice for discussing risks with patients: “Both [general practitioners] and rheumatologists should educate their PMR patients about the main cranial symptoms and signs of GCA, while stressing the low frequency of such an occurrence so as not to worry them unnecessarily. No additional testing is needed, since both PMR and GCA flares are best diagnosed upon raised ESR and CRP, along with a complete blood count.”
Kimberly J. Retzlaff is a freelance medical journalist based in Denver.
References
- Liozon E, de Boysson H, Dalmay F, et al. Development of giant cell arteritis after treating polymyalgia or peripheral arthritis: A retrospective case-control study. J Rheumatol. 2018 Mar;45(5):678–685.