Sulfaslazine and Hydroxychloroquine
These have been reported to improve JIA, but there are no reports of inactive disease or remission. Sulfaslazine may be particularly useful in those with oligoarthritis or those with enthesitis-related disease. With the availability of biologic therapies, these are not used as frequently today.
Systemic Onset JIA
Systemic onset JIA (SJIA) deserves special discussion because it presents unique challenges including establishing a correct diagnosis and treating persistent severe disease and MAS. A correct diagnosis is crucial because prednisone treatment prior to treatment for a childhood malignancy can decrease the response to chemotherapy and, consequently, survival.
Nearly all children with SJIA will need steroid therapy for treatment of the systemic features. If articular features predominate and there are few or no systemic features or MAS (see below), MTX and/or anti-TNFs can be effective. For patients with both arthritis and systemic features/MAS (or if the latter predominate), cyclosporine and anti-IL1 therapy may be needed. Despite aggressive therapy, about 20% of children with SJIA will have disease that does not respond to these treatments. For these children, there are anecdotal reports of response to combination anti-IL1 and anti-TNF therapy, thalidomide, cytoxan, etoposide, and rituximab. With each of these medications, there is tremendous worry about side effects and need for special surveillance for infection, toxicity, and long-term adverse effects.
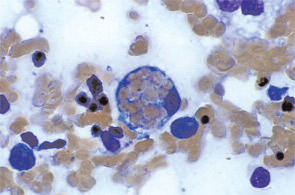
Macrophage Activation Syndrome
MAS is the result of overactive macrophages. This condition has been reported in many pediatric rheumatic diseases but occurs with greatest frequency in SJIA either at disease onset, with a flare, or during persistently active disease. MAS presents with a wide spectrum of symptoms and laboratory abnormalities that many clinicians feel may be an integral part of SJIA, rather than a separate event.5 Patients with early, mild MAS may have only mild laboratory abnormalities and active systemic disease while others are critically ill in the intensive care unit with persistent rash, persistent high fevers, central nervous system dysfunction, hemorrhagic abnormalities, and cardio-pulmonary-renal failure. Laboratory abnormalities of MAS reveal increasing C-reactive protein (CRP), d-dimer, ferritin, lactate dehydrogenase, aspartate aminotransferase, prothrombin time, and partial thromboplastin time with falling erythrocyte sedimentation rate (ESR), hematocrit, platelets, white blood cell count, and fibrinogen. Mild abnormalities may respond to treatments initiated for the SJIA. However, if abnormalities worsen, then prompt use of high-dose pulse IV solumedrol and IV cyclosporine are important to halt this potentially fatal process.6
Summary
In conclusion, no one combination of medications has been shown to be fully effective in treating JIA. With what is known to date, the most effective approach for many children may be prednisone (and/or intra-articular steroids), MTX, and an anti-TNF agent at the time of diagnosis to rapidly squelch disease. Once remission has been achieved medications can slowly be decreased to a maintenance regimen. Future research will hopefully provide the insights and tools to identify which patients will rapidly achieve remission with lesser therapies.