The brain biopsy is “particularly important,” Dr. Birnbaum said.
“The role of a brain biopsy is not only to secure the diagnosis of a primary angiitis of the central nervous system, but also potentially uncover occult CNS mimics,” he said.
CNS Syndromes in NPSLE
Dr. Birnbaum described a three-step process for diagnosis and treatment of NPSLE: identifying whether a CNS syndrome is due to SLE or another co-morbidity; defining the spectrum of the syndrome; and understanding when to use immunosuppressive treatment rather than symptomatic treatment.
A key point, he said, is to “always suspect that, when you have a lupus patient presenting with neurological complications, that neurological disease is not attributable to lupus.” Up to 40% of SLE patients will have a CNS syndrome not due to SLE.1 It’s important to be aware of the “lurking possibility of an infection,” he said.
“The differential diagnosis can be vast,” he said. “You can formulate a very, very comprehensive differential diagnosis using a mnemonic called VITAMIN.” This, he joked, was a distillation of three years of neurology residency into one slide.
VITAMIN
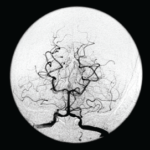
- Vascular/stroke: These include septic emboli, subarachnoid hemorrhage from mycotic aneurysms, septic thrombophlebitis;
- Infections: These should be classified as bacterial, fungal or viral source and by anatomic region, whether parenchymal, meningeal or vascular;
- Traumatic: This just means the experience is traumatic for the patient and is not very relevant to the diagnosis, Dr. Birnbaum said;
- Autoimmune or inflammatory syndromes;
- Metabolic: This includes derangements from renal insufficiency or posterior reversible encephalopathy syndrome (PRES);
- Iatrogenic: Complications, potentially from corticosteroid or immunosuppressive therapy; and
- Neoplastic causes.
He hammered home the point that “none of these causes, obviously, from competing co-morbidities, require immunosuppressive therapy.”
Once competing co-morbidities are excluded, the clinician has to assess whether the syndrome is seen more frequently in lupus than in non-SLE controls, he said. Headache, mood disorders, anxiety disorder and mild cognitive impairment are syndromes seen with similar frequency within lupus and without, and can be dealt with as though the patient does not have lupus. Treatment should not include immunosuppressants, Dr. Birnbaum said.
Once a syndrome is actually determined to be neuropsychiatric SLE, the clinician has to decide whether to use immunosuppressants.
But, he said, in the absence of extra-neurological activity, immunosuppressants are rarely warranted—not in the case of cerebrovascular disease, which is seen in 5–15% of SLE patients; not for seizures presenting later into the SLE course, with seizures seen in 5–20%; not in cognitive impairment, seen in up to 80% of SLE patients; and usually not in psychosis, which is seen in up to 5% of patients.