Presentation
“Patients with small fiber neuropathy classically complain of burning and stinging dysesthesia in the feet that is worse at night and aggravated by prolonged standing or walking,” says Dr. Polydefkis. The onset is indolent, symmetric and painful, and is most commonly length dependent.
He would expect a patient with an isolated small fiber neuropathy to have normal strength, normal reflexes and normal vibration thresholds. “If any of these are abnormal, this is likely not a small fiber neuropathy,” he says.
Given small fiber regulation of autonomic function, patients may also present with changes in sweating, urination and bowel function.
Evaluation
Evaluation for suspected small fiber neuropathy consists of a thorough history, examination and diagnostic testing. Small fiber neuropathy is idiopathic in 50% of cases, but most commonly is due to diabetes mellitus.3 Dr. Polydefkis recommends evaluating for vascular risk factors, such as diabetes, hypercholesterolemia and hypertension, nutritional deficiencies and other metabolic causes, such as hypothyroidism and cancer. Toxic exposures, such as chemotherapy, excess pyridoxine and immune modulators, are also common causes, and if a family history of neuropathy exists, inherited causes should be considered.
Among the rheumatic etiologies, small fiber neuropathy is most commonly seen in Sjögren’s disease, and has also been demonstrated in sarcoidosis, systemic lupus erythematosus (SLE) and scleroderma. In patients with Sjögren’s disease, neurologic symptoms may precede the diagnosis of Sjögren’s. Notably, Sjögren’s disease is associated with several disorders of the peripheral nervous system, and small fiber neuropathy is among the most common. Patients with small fiber neuropathy and Sjögren’s are more commonly seronegative and, thus, lack anti-SSA and anti-SSB autoantibodies.4
In several studies, small fiber neuropathy has also been demonstrated in patients with fibromyalgia.5 “This is an evolving area,” says Dr. Polydefkis, and “those studies tended to have small sample sizes. Further work is needed.”
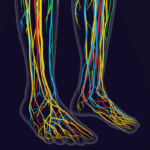
Diagnostic testing for peripheral neuropathy often begins with a nerve conduction study. However, in small fiber neuropathy, nerve conduction study results will be normal given that the lightly and unmyelinated small nerve fibers result in conduction beyond the resolution of the test.2 Diagnostic confirmation requires a cutaneous nerve biopsy, performed via a punch biopsy. The specimen is examined for intra-epidermal nerve fiber density (IENFD), which is considered abnormal when reduced, particularly when less than the fifth percentile.3
In practice, Dr. Polydefkis often performs skin biopsies at “proximal and distal sites along the leg. Standard sites have been established and normative values have been published. Because most forms of peripheral neuropathy affect the distal terminals of the longest nerve fibers, the distal leg site is the most sensitive to detect small fiber neuropathy.” In non-length-dependent small fiber neuropathy, the intraepidermal nerve fiber density may be abnormal in skin from proximal sites with normal distal biopsy findings.