 In patients with Takayasu arteritis (TAK) who are resistant to conventional treatments and tumor necrosis factor-alpha (TNF-α) inhibitors, the Janus kinase (JAK) inhibitor baricitinib demonstrated an effective treatment response and decreased glucocorticoid use, according to results from a small study published in Rheumatology. The study also found no serious adverse events related to baricitinib.1
In patients with Takayasu arteritis (TAK) who are resistant to conventional treatments and tumor necrosis factor-alpha (TNF-α) inhibitors, the Janus kinase (JAK) inhibitor baricitinib demonstrated an effective treatment response and decreased glucocorticoid use, according to results from a small study published in Rheumatology. The study also found no serious adverse events related to baricitinib.1
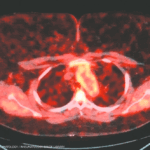
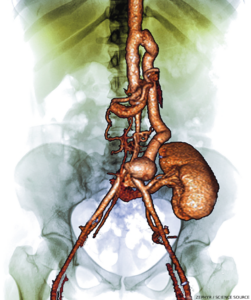
“Takayasu arteritis is a form of vasculitis primarily affecting the aorta and its major branches. It predominantly occurs in young adults, and if poorly managed, it poses a significant threat to long-term outcomes and quality of life, and can lead to a loss of social productivity,” explains the study’s lead author Jiachen Li, MD, a rheumatologist in the Department of Rheumatology and Immunology at Peking University People’s Hospital, Beijing.
“TNF-α inhibitors serve as a key therapeutic option when conventional treatments fail. However, a subset of patients does not achieve remission even with TNF-α inhibitor therapy. Therefore, exploring new and effective treatment strategies for this [subset of] Takayasu arteritis refractory to TNF-α inhibitor is of critical importance,” notes Dr. Li.
“Our clinical trial demonstrated that in patients with TNF-α refractory Takayasu arteritis, 80% of the study participants achieved either complete or partial remission after 24 weeks of baricitinib treatment,” Dr. Li says. “We also observed a marked reduction in systemic inflammation and corticosteroid dosage by patients. Further, no disease relapse or serious adverse events were recorded during the 48-week follow-up period.”
Efficacy & Safety Study
Researchers conducted the prospective, single-arm study between February 2021 and August 2023 across three hospitals in China. The study evaluated the efficacy and safety of baricitinib in 10 adults with TAK, based on the 1990 ACR criteria for TAK, refractory to TNF-α inhibitors, glucocorticoids and at least one additional immunosuppressant. Previous TNF-α inhibitor treatment included adalimumab in six patients, etanercept in three patients and infliximab in one patient. Immunosuppressive regimens included mycophenolate mofetil in four patients, methotrexate in two, azathioprine in two, cyclophosphamide in one and a combination of leflunomide and tacrolimus in one patient. The median age of the nine female patients and one male patient was 29 years, and the median disease duration stood at 56.5 months.
After discontinuing the TNF-α inhibitors for a washout period, the patients received 4 mg of baricitinib daily for 48 weeks, in addition to glucocorticoids and immunosuppressants. Along with clinical and laboratory assessments, patients underwent vascular ultrasound and computed tomography angiography. The primary end point was overall response rate, comprising complete remission plus partial remission, at 24 weeks.
The secondary end points included changes from baseline in the following disease activity scores: the National Institutes of Health (NIH) score, the Indian Takayasu Clinical Activity Score (ITAS2010) and the Indian Takayasu Clinical Activity Score with acute-phase reactants (ITAS-A). Secondary end points also included changes from baseline levels of erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), glucocorticoid doses from baseline to 24 weeks, the relapse rate by 48 weeks among patients who attained remission and the incidence and severity of adverse events.
Remission Reached
The overall response rate at 24 weeks stood at 80%, with eight patients achieving remission: Six patients achieved complete remission and two experienced a partial remission. The remaining two patients experienced disease progression, comprising headache and worsening of renal and carotid arteries stenosis in one patient and fever, elevated blood pressure and renal artery stenosis progression in another.
Disease activity scores improved for all 10 patients at 24 weeks. When compared with the median baseline scores of 3.0 for NIH, 5.0 for ITAS2010 and 6.5 for ITAS-A, the 24-week scores all reached zero. The inflammatory markers also improved for all patients at 24 weeks. The mean baseline ESR of 26.5 mm/hr fell to 3.5 mm/hr, and CRP went from 34.4 mg/L to 3.3 mg/L at week 24.
Imaging studies suggested that six patients experienced no vascular disease progression at 24 weeks, compared with baseline; one patient showed improvement in her subclavian artery stenosis, and one patient showed improvement in her carotid artery stenosis. The median dosage of glucocorticoids decreased from 20.0 mg/day at baseline to 6.3 mg/day at 24 weeks. At 48 weeks, the eight patients who achieved remission by week 24 did not relapse. Disease activity, inflammatory markers and glucocorticoid doses did not differ from the 24-week assessments.
During the 48-week follow up, two patients developed upper respiratory tract infections and one patient experienced diarrhea. The patients recovered with anti-infective and symptomatic treatment. The study recorded no serious adverse events, including major cardiovascular events, thromboembolism, opportunistic infections or severe allergic reactions.
Clinical Implications
“Currently, when patients with Takayasu arteritis respond inadequately to TNF-α inhibitor therapy, clinicians may escalate the dose or frequency of the TNF-α inhibitor, or augment therapy with corticosteroids or immunosuppressants. However, these strategies often increase the risk of adverse drug reactions,” Dr. Li says. “The findings of our study offer a new therapeutic alternative for managing refractory Takayasu arteritis. Baricitinib may represent an effective and safe treatment option in cases of suboptimal response to TNF-α inhibitors, which is of significant importance for improving patient outcomes.
“Our findings indicate that baricitinib not only alleviates clinical symptoms but also significantly reduces systemic inflammatory markers,” Dr. Li continues. “Further, its steroid-sparing effect is of considerable importance for improving long-term patient outcomes.”
Still, Dr. Li notes that “this trial included only 10 patients with TNF-α inhibitor-refractory Takayasu arteritis. The small sample size necessitates further validation of our conclusions through larger, two-arm studies in the future.”
Randomized, Controlled Trials Needed
Haner Direskeneli, MD, chief of rheumatology at Marmara University School of Medicine in Istanbul, notes, “There are two open-label case series of baricitinib use in refractory TAK. Both included 10 patients, with overall response rates at 24 weeks of 80% in the study by Li et al. and 60% in the study by Zhou et al. There was one withdrawal due to toxicity among 20 patients.2 These data are promising, but need to be confirmed by prospective controlled trials.
“The definition of refractory TAK is not clear and validated, but most patients get biologics (either TNF blockers or tocilizumab) when glucocorticoids plus conventional immunosuppressives (methotrexate, azathioprine, mycophenolate or leflunomide) fail,” Dr. Direskeneli continues. “JAK inhibitors can be an option in patients who are refractory or intolerant to biologics. In this group, secukinumab is also promising.”
Dr. Direskeneli adds, “Among JAK inhibitors, tofacitinib has more data (case series and comparative, open-label, prospective studies with methotrexate and leflunomide) with also good results. So either baricitinib or tofacitinib can be used. There is a finished randomized, controlled trial of upadacitinib, but the results are not reported yet.”3
Concluding, Dr. Direskeneli says, “Unfortunately, TAK is an orphan disease and most data come from case series or open-label, comparative studies. As expected, the efficacy data is usually quite good. However, unless we have randomized, double-blind, placebo-controlled trials, it is not satisfactorily clarified how much efficacy (and toxicity) new agents have.”
Katie Robinson is a medical writer in New York.
References
- Li J, Xia W, Ji H, et al. Baricitinib for Takayasu arteritis refractory to TNF-α inhibitors: A multicentre, single-arm trial. Rheumatology (Oxford). 2025 Oct 1;64(10):5262–5268.
- Zhou Z, Fang C, Wang L, et al. Baricitinib for refractory Takayasu arteritis: A prospective cohort study in a tertiary referral centre. RMD Open. 2024 Mar 22;10(1):e003985.
- A study to evaluate the efficacy and safety of upadacitinib in participants with Takayasu arteritis (TAK) (SELECT-TAK). Clinical trial NCT04161898. 2025 Aug 14.