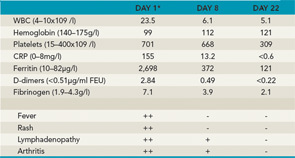
Key: ++=severe, +=moderate, -=absent *Baseline before treatment with anakinra.
Typical Disease Progression
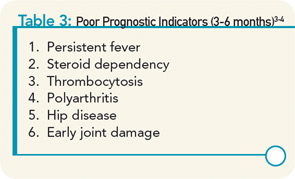
Despite the protean presenting manifestations of the disease, up to 40% of children have a good long-term outcome with a monocyclic course that enters a permanent remission after a variable number of months. A small number of patients have a polycyclic course with recurrent episodes of active disease and periods of true remission, while more than half of the patients have a more severe, persistent disease course. Prognostic markers of poor outcome have been identified, but do not have optimum sensitivity or specificity (see Table 3).3,4 Among the group with persistent disease, the most severely affected children have ongoing systemic symptoms, early destructive polyarthritis, growth failure, and all the attendant side effects of chronic systemic corticosteroid treatment, on which children are often dependent to maintain a reasonable level of physical activity and quality of life. Traditional disease-modifying antirheumatic drugs (DMARDs), such as methotrexate, have limited efficacy for the joint disease and virtually no impact on the systemic features of the disease.
In addition to the disease-related complications in the acute phase, such as serositis, severe anemia, and MAS, and the devastating consequences of the polyarthritis of sJIA, treatment-related complications have resulted in major morbidity in this population. Until recently, many patients required relatively large doses of corticosteroids to control systemic disease, articular disease, or both. In fact, in some patients, treatment-related morbidity has been worse than disease-related morbidity. This has been observed in two particular areas where steroid treatment has been additive to disease-related manifestations. Growth delay is commonly observed and is certainly more prevalent in patients with worse disease requiring more treatment. Several studies have reported the use of growth hormone (GH) resulting in improved linear growth.5 However, there is still controversy regarding whether these children have an improved final height or whether their growth is only accelerated during the time that the GH is being administered.6 Secondly, steroid- and disease-related osteopenia and osteoporosis can have serious consequences, including pathologic fractures; if these involve the vertebral bodies, final height may also be impacted. The pain from the fractures also results in immobility, further accelerating the development of osteopenia. Medications other than corticosteroids are needed to reduce—or, in fact, prevent—these severe complications.
Treatment Advances
Advances in the understanding of the disease pathogenesis have resulted in the application of biologic treatments directed at inhibiting cytokines associated with the disease, particularly interleukin (IL) 1 and IL-6. Recent studies suggest that targeting these specific cytokines may result in much better outcomes than treating with corticosteroids and traditional DMARDs and may avoid the devastating toxicity of high-dose corticosteroid treatment.