The underlying tenet of the ACR’s advocacy efforts is that we cannot effect change for our profession and our patients unless we take our issues directly to decision makers. As I write this column, I am highly encouraged by the progress we have made so far this year in the advocacy realm. At the same time, developments on a daily basis remind me we cannot rest on a sense of accomplishment. In fact, significant new policy discussions have arisen, particularly around drug pricing, that will require each of us in the rheumatology profession to stay vigilant and involved to ensure our patients’ access to care is protected.
In February, I wrote about the persistent challenges we face in rheumatology, with specific attention to the most pressing potential hazards we faced at that time. This included a change by the Centers for Medicare & Medicaid Services (CMS) that would have adjusted reimbursements for Part B drugs based on the prescribing provider’s performance in Medicare’s Merit-Based Incentive Payment System (MIPS).
Thanks to the advocacy efforts of countless ACR/ARHP members and our partner specialty societies, Congress implemented our requested legislative fix to ensure this ill-conceived change would never happen. Better yet, in the same piece of legislation that fixed our issue with MIPS and Part B drugs, Congress permanently repealed the annual cap on therapy payments, closed the Medicare Part D donut hole one year early, finally repealed the Independent Payment Advisory Board (IPAB), and provided $2 billion in funding for the National Institutes of Health (NIH). Thus, a feeling of accomplishment is justified.
Congressional Meetings

Rep. Burgess
In May, during our annual Advocacy Leadership Conference and Capitol Hill visits, a team of close to 100 ACR/ARHP leaders traveled to Washington, D.C., to promote rheumatology priorities. While there, we had a chance to thank lawmakers for this work, share concerns about additional challenges and make the case for assistance on other key issues. During the conference, we were joined by Rep. Michael Burgess, MD (R-TX), who was responsible for shepherding many of these legislative successes through Congress. Rep. Burgess said we need to stay persistent and keep engaging with policymakers on the major issues and proposals that will affect all of us and our patients.
This is a central question for us in rheumatology now. As responsive as policymakers have been, major policy discussions are taking place now that require all of us in the field of rheumatology to get involved personally. We need to educate policymakers and, in the process, protect our patients’ access to care and treatment, and the specialty itself.
Major relevant examples include proposals to rein in high drug prices for patients, a goal the ACR shares with policymakers and others. The ACR strongly believes that safe and effective treatments should be available to patients at the lowest possible cost. Unfortunately, many of the efforts by payers to lower drug expenses result in reduced access to effective and affordable treatments for patients that need them. The College has put forward a number of proposed policies that would bring down drug costs for patients while protecting patient access to treatments. These include:
- Requiring plans to apply a substantial portion of rebates at the point of sale;
- Establishing a beneficiary out-of-pocket maximum in the Medicare Part D catastrophic phase to provide beneficiaries with better protection against high drug costs;
- Decreasing concentration in the pharmacy benefit manager (PBM) market and other segments of the supply chain;
- Increasing transparency in how pharmaceutical companies, pharmacy benefit managers and health insurance companies determine the cost of prescription medications;
- Increasing transparency of any incentives given by drug companies to pharmacy benefit managers or health insurance companies related to the dispensing or promotion of their manufactured drugs;
- Eliminating excessive patient cost sharing usually required by formularies’ specialty tiers or providing an expeditious exception and appeal process for Part D beneficiaries who are affected by specialty tier practices; and
- Allowing Medicare to negotiate with pharmaceutical companies to achieve more affordable drug pricing.
Trump’s Plan
In May, the U.S. Department of Health and Human Services (HHS) released a request for information (RFI) related to the Trump administration’s blueprint to lower drug prices and reduce patients’ out-of-pocket costs. The ACR agrees that action on high drug prices is long overdue, and we were pleased to see the inclusion of proposals that would create PBM pricing transparency, promote biosimilar development and reduce out-of-pocket costs in Part D. However, we were concerned that several proposals—particularly allowing Part D plans to further restrict drug formularies and moving Part B drugs into Part D—could make it more difficult for our patients to access needed therapies. The ACR is closely analyzing these proposals as we develop a comprehensive response to the RFI ahead of the July deadline for comments.
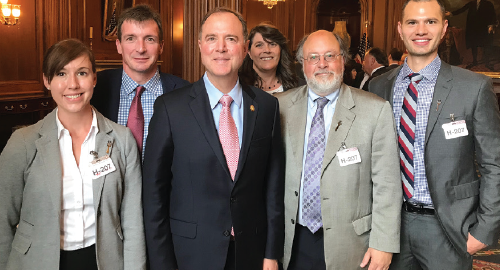
ACR President David Daikh, MD, PhD, with
Rep. Adam Schiff (D-CA-28) and California rheumatology advocates. From left: Christina Downey, MD; William Robinson, MD, PhD; Rep. Schiff; ARHP President Sandra Mintz, MSN, RN; Dr. Daikh; and Matthew Baker, MD.
When these proposals on drug pricing were introduced, it was immediately clear that our advocacy and education of policymakers would again be critical. We share the administration’s and HHS’s goal to provide patients with high-quality, cost-effective treatment, but we need to remain vigilant and engaged so proposals to reduce patient costs do not weaken or inhibit access to care and our ability to prescribe the right therapy for a patient.
With an issue as complex as drug pricing, it is much more likely that efforts to create a universal a solution will miss the mark for some specialties and patients. This was abundantly clear as we began reviewing proposals and comments by administration officials. For example, it appears policymakers are focusing on incentivizing use of lower-cost therapy options, even if it is through policies that penalize use of high-cost therapies.
This is concerning for the rheumatology community because providers don’t have equally effective, less expensive alternative therapies to choose from. Generally, when a rheumatologist reaches for a biologic therapy, the patient has already failed a less expensive therapy, and we know the biologic therapies our patients rely on to control their disease can be life changing. We and our patients have a narrow range of treatment options, and the costs associated with these treatments do not vary widely, but many policymakers may not be aware of this fact. We must educate policymakers as part of our advocacy efforts.
There also appears to be a lack of understanding of the nature of the barriers our patients face when it comes to the utilization management techniques used by PBMs and payers in the commercial and Medicare Part D spaces. Step therapy, or fail-first requirements, in Part D and commercial plans are among the practices that delay patients getting the right treatment when they need it. When a patient is granted access to a requested therapy, the out-of-pocket costs for patients are often very high or literally unaffordable for RA patients.
Yet these barriers are overlooked in proposals to move the therapies currently in Part B—where these hurdles are not usually an issue—into the Part D structure, in which patients currently experience significant access to treatment challenges. The proposal may seem to make sense to policymakers who believe PBMs and others can manage these drugs and formularies in a way that produces cost savings. It may not be obvious to them that patient access to the treatments they need may be jeopardized if this happens and the challenges with Part D are not addressed. It is paramount that the quest for savings does not take priority over patient access and standard of care in rheumatology practice. How will policymakers know about this nuance if we don’t get involved?
Call to Action
I want to personally thank all ACR and ARHP members who take the time to reach out to lawmakers, as well as those who stay engaged with the ACR/ARHP by volunteer involvement or by letting us know the challenges you face in your practice. Hearing from you allows us to better identify and frame the issues for policymakers. You can contact your lawmakers through our Legislative Action Center—writing them on a number of important preselected issues with suggested messaging or simply using the portal to send your own individual concerns—and you can contact your advocacy team at [email protected] with policy concerns or help building on your own advocacy efforts.
These days, the need for personal outreach from all of us only seems to grow. It’s important that we all continue to engage and educate those who are making decisions on our behalf on the issues that impact our specialty and our patients. As Rep. Burgess asked, “If we don’t advocate for rheumatology and for our patients, who is going to do that?”
Learn how RheumPAC can help advance our issues in D.C. Go to www.rheumatology.org/advocacy.
David I. Daikh, MD, PhD, is the 81st ACR president. Dr. Daikh serves as the director of the Rheumatology Fellowship Training Program at the University of California, San Francisco and as chief of the Rheumatology Division at the SFVA Medical Center, where he directs the Rheumatology Clinic.


