Unlike biopsy, repeat ultrasound can provide prognostic value. OMERACT developed the GCA ultrasound score (OGUS), which has demonstrated that higher scores at baseline portend higher risk of relapse in one year and decreases in scores after treatment are associated with decreased risk of relapse.8,9
Dr. Schmidt shared his success with GCA fast-track clinics, including their impact on reducing visual impairment.10 He outlined benefits of establishing fast-track clinics, such as easy and rapid appointment scheduling, and recommendations, such as use of appropriate technology, including ultrasound probes with a frequency of at least 18 MHz, and collaborating with ophthalmologists, neurologists and radiologists for imaging, such as magnetic resonance imaging (MRI) and PET-CT, as well as with surgeons to pursue biopsy if needed. The main barrier to entry, however, is his recommendation to have performed at least 50 ultrasounds of the temporal and axillary arteries—and ideally over 300.11
Dr. Schmidt closed with a convincing list of positive attributes for TAUS: It’s widely available. There’s no need for a referral. It is integrated into the exam, fast, cost effective, patient friendly, high resolution, able to detect subclinical GCA in PMR and and repeatable—supported by excellent evidence. Perhaps most convincingly, he emphasized how fun and satisfying it can be to provide patients with an immediate answer to their concerns.
Ultrasound Should Not Replace Biopsy for GCA Diagnosis
The counterargument was presented by Tanaz Kermani, MD, MS, professor of medicine and founder and director of the Vasculitis Program at the University of California, Los Angeles. Dr. Kermani presented on behalf of Peter Grayson, MD, MSc, senior investigator at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), who was unfortunately unable to attend given the government shutdown at the time of ACR Convergence 2025.
Dr. Kermani conceded that ultrasound has its benefits, particularly that it is safe and cost effective and can be performed at the bedside. However, she noted that suspected diagnoses must be confirmed, that we should be particularly careful to avoid false positives, and that this is best done with biopsy.
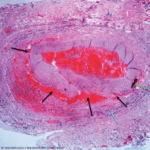
She identified histology as the gold standard, with 100% specificity, and noted that other diseases, such as atherosclerosis and other forms of vasculitis, can cause the halo sign, leading to risk of misclassification as GCA. She also argued that the sensitivity of the halo sign, between 70 and 78%, was unsatisfactory and could lead to missed diagnoses of GCA.