To illustrate this point, she presented the case of a 61-year-old man with a new diagnosis of GCA. He had experienced constitutional symptoms for five weeks, jaw claudication and new-onset fronto-temporal headache. Inflammatory markers were elevated and ultrasound demonstrated bilateral halo sign of the temporal arteries. His symptoms and inflammatory markers improved when he was taking 40 mg of prednisone; however, his symptoms returned upon tapering to 30 mg. He underwent temporal artery biopsy, which was negative. Upon referral to the National Institutes of Health (NIH) for a second opinion, urinalysis demonstrated red blood cell casts and serologic testing demonstrated positive anti-myeloperoxidase antibodies. He underwent kidney biopsy and was diagnosed with anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis with pauci-immune glomerulonephritis.
Dr. Kermani outlined a framework for assessing GCA on the basis of low, intermediate and high pre-test probability, pointing out that ultrasound is most useful on both extremes of the spectrum: a negative study in a low-probability patient or a positive study in a high-probability patient.12 In instances with greater uncertainty or discordant findings, temporal artery biopsy can serve as the decisive test.
She pointed out that the data for use of ultrasound in GCA originate from expert centers, but many GCA cases are diagnosed by internists or in non-expert centers. “Yes, if you’re Wolfgang Schmidt doing an ultrasound, you don’t need a biopsy, but what about the rest of us? Expertise should dictate your diagnostic approach.”
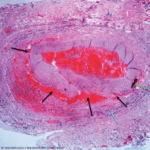
Dr. Kermani provided important recommendations to increase the yield of temporal artery biopsy: they should be 2–3 cm in length, obtained in a timely manner and reviewed directly with the pathologist. Red flags suggestive of an alternative diagnosis include lack of granulomatous inflammation, as well as the presence of fibrinoid necrosis or eosinophils. To close, she noted that evaluation for GCA usually involves more than one diagnostic modality and that rheumatologists should be familiar with them all.
Q&A & Closing Thoughts
During the Q&A section, one attendee expressed concern that temporal artery ultrasound is often performed by technicians without standardized protocols and subsequently read by radiologists without expertise in GCA. Dr. Schmidt whole-heartedly agreed, and recommended rheumatologists spearhead training efforts and establish protocols for vascular imaging. Another attendee also commented on the challenges of obtaining expertise in performing temporal artery ultrasound in the U.S., arguing the debate itself is somewhat artificial and the preference for one study over another is largely based on regional expertise.