The new criteria have not given exact definitions for some of the variables, a situation that may lead to confusion or contention. First, according to the new criteria, if a patient has joint erosions in the context of an inflammatory condition, he or she can be classified as having RA without fulfilling any of the other criteria. Erosive disease is not defined. Is an erosion defined as a broken cortex? Or is a subchondral cyst with an intact cortex, which may precede the development of a lesion with broken cortex, identified as an erosive state as well? Is the localization of erosiveness relevant? In addition, is one erosion enough for the definition of RA, or should a number of erosions be present to be sure that true erosive disease is present?
There are recent data on the prognostic value of baseline erosions in patients presenting with UA. Thabet et al show that the presence of one erosive joint has a limited predictive value for development of RA, according to the ACR criteria and persistent disease.5 The presence of two, three, or four erosive joints had an equivalent positive predictive value; if five or more erosions were present, the predictive ability was further increased. From these data, one can conclude that the term erosive disease would entail the presence of at least two erosive joints. Surprisingly, the presence of two erosive joints at first presentation to the early arthritis clinic is no guarantee of a persistent disease course. Of patients with two erosions, 32% achieved a spontaneous remission.4
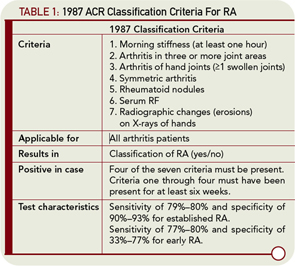
These data are in contrast to the significance of baseline erosions in patients with RA (by the 1987 ACR criteria); in these patients, the presence of erosions at baseline is the most powerful prognostic factor for a destructive disease course. This finding underlines the notion that UA contains a much more heterogeneous set of patients than established RA. If the findings of Thabet et al can be replicated in another set of UA patients, this information might be considered in the definition of erosiveness. Indeed, it may raise the question as to whether the presence of erosiveness in patients with early UA is so specific and predictive that no other criteria need to be met to diagnose RA.
The second variable that needs to be clarified in the new criteria is the definition of a high level of RF and a high level of ACPA. There are some data that support the notion that high levels of these autoantibodies have an increased specificity and predictive value compared with low levels. An important issue relates to the appropriate cut off for a high level of these autoantibodies. Establishing a working definition could be problematic because of the variety of available methods for autoantibody measurement. The most common methods are ELISAs. These assays are characterized by differences in performance features such as the standard curves, cut-off values for positivity, and maximal levels. For instance, some RF kits have a reference for positivity of >5 units, whereas in other kits this is 25 units. This means that a level of ≥50 is a moderately elevated level using the latter kit but is a markedly increased level in the former kit. Moreover, the day-to-day variation in assay performance is often considerable. A modest correlation between RF levels determined with different ELISAs and nephelometers in the same sera has been described.6 Differences in identifying a high RF or ACPA level could therefore complicate the application of the new ACR/EULAR criteria and lead to differences in the readiness to diagnose RA between sites.