WASHINGTON, D.C.—As of November 2024, there are 16 biologic disease-modifying anti-rheumatic drugs (bDMARDs) that are FDA approved for the treatment of psoriatic arthritis (PsA). Incredible news, right? But as my fellowship program director used to say, “There’s no free lunch.” This buffet of options is excellent for our patients, but poses challenges to the practicing rheumatologist when it comes to treatment selection.

Ana-Maria Orbai, MD, MHS
In the ACR Convergence 2024 Review Course, Ana-Maria Orbai, MD, MHS, director, Psoriatic Arthritis Program, and associate professor of medicine, Division of Rheumatology, Johns Hopkins University School of Medicine, Baltimore, provided a practical framework for choosing drugs for our patients with PsA. Treatment recommendations were based on the most recent EULAR and Group for Research and Assessment of Psoriasis and PsA (GRAPPA) guidelines. These guidelines overlap in most places, but do differ slightly in others.1,2
Treatment Choice Depends on PsA Domains
As with most diseases we manage as rheumatologists, PsA looks different for every person who has it. Clinical heterogeneity is the norm, and different patients respond better to some drugs than others. Therefore, thinking about PsA treatment through the lens of domains—that is, specific manifestations of disease—allows us to better tailor therapy selection. The domains of PsA include:
1. Axial PsA. Axial inflammation in PsA differs from that of axial spondyloarthritis (SpA). Prevalence increases with disease duration, and sacroiliitis tends to be asymmetric. What’s more, HLA-B27 positivity, inflammatory back pain and syndesmophytes are less common in axial PsA than in axial SpA.3
Dr. Orbai noted, “It’s important to determine if patients have this because [axial inflammation] will reduce our treatment options to tumor necrosis factor inhibitors (TNFi), Janus kinase inhibitors (JAKi), and interleukin-17 inhibitors (IL-17i).” IL-12/23i and IL-23i are notably missing from this list, although studies are ongoing for IL-23i in axial PsA.
EULAR and GRAPPA guidelines recommend four weeks of non-steroidal anti-inflammatory drugs (NSAIDs) and physical therapy, with escalation to bDMARDs if the patient hasn’t improved.
2. Dactylitis. Dactylitis is seen in about 50% of patients with PsA—the most of any spondyloarthritis. Dr. Orbai reminded us, “Acute dactylitis is associated with tenderness, not just swelling and purplish discoloration. Chronic dactylitis involves swelling without tenderness and discoloration.”
Many more treatment options are reasonable when it comes to dactylitis, compared with axial PsA, with IL-12/23i, IL-23i, and possibly phosphodiesterase 4 inhibitors (PDE4i) added to those listed above.
3. Enthesitis. “The agreement between clinical and sonographic enthesitis is low overall, and it’s slow to respond to treatment,” Dr. Orbai noted.4 A recent post-hoc analysis of secukinumab (IL-17i) vs. adalimumab (TNFi) for enthesitis showed similar efficacy and time to resolution, with a median time to resolution of 85 days.5 Treatment recommendations mirror those for dactylitis above.
4. Psoriasis & Nails. Dr. Orbai highlighted a 2023 Cochrane review that helped identify the most effective bDMARDs for skin disease. IL-17i, IL-23i and infliximab (an intravenous TNFi) cleared skin most efficaciously.6
Dr. Orbai noted, “I also want you to be aware of studies looking at bDMARD choice and the onset of PsA in patients with psoriasis.” A retrospective cohort study showed a lower hazard ratio for the development of inflammatory arthritis in patients with psoriasis treated with IL-23i than for TNFi and IL-17i.7 However, ongoing studies are needed to definitively determine if certain bDMARDs can delay (or better yet, prevent) the development of PsA in people with psoriasis.
5. Peripheral Arthritis. “The common stem for inflammatory arthritis is going to be a TNFi, IL-17i, IL-23i or JAKi,” Dr. Orbai noted. Conventional synthetic DMARDs like methotrexate may also be useful but are not necessarily always first-line options.
6. Symptoms & Life Impact. Lastly, we can’t forget that treatment success is dependent on both suppressing inflammation and managing the patients’ experience. Patient pain, fatigue, stiffness and functioning are additional factors to consider.
Which Biologic to Choose?
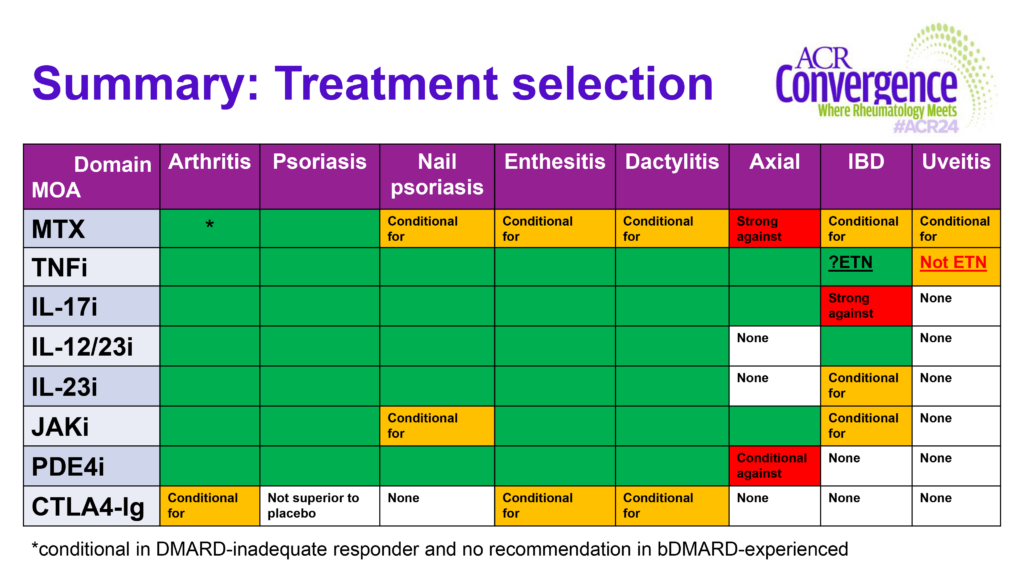
So when all is said and done, which bDMARD should we use choose first? Dr. Orbai offered, “Consider a patient’s worst domain, as well as each specific domain of disease that’s involved. Then, aim for the maximum domain coverage and the most effective bDMARD choice.”
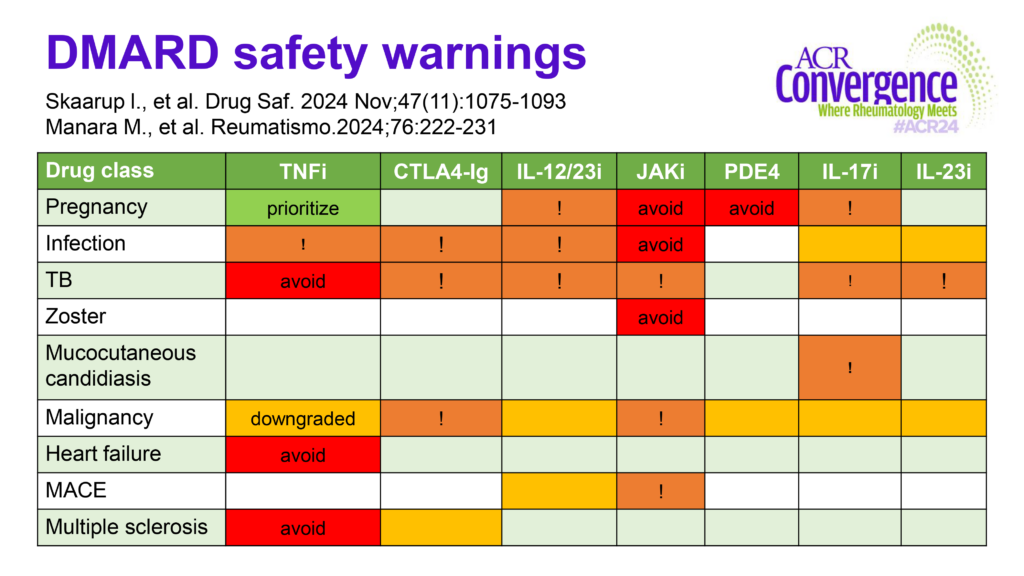
Even after identifying a patient’s disease domains, a lot of treatment options may remain. “A good way to narrow options for a patient is based on DMARD safety warnings,” Dr. Orbai noted. Some drugs confer higher risks to certain patients than others, so aim to maximize benefit while minimizing risk.
Dr. Orbai was kind enough to share two amazing tables from her talk that “took a long time to make.” Figure 1 divides treatment options up by disease domain and combined recommendations from EULAR and GRAPPA, and Figure 2 summarizes safety concerns.
What Would Dr. Orbai Do?
So how does Dr. Orbai think about her patients when it comes to choosing therapy? To guide her choice, she always defines:
- The target tissue(s)/domains affected;
- New manifestations of disease vs. reactivation;
- The patient’s prior treatment history and responses;
- The patient-reported outcome (PRO) profile: disease impact and symptom experience; and
- Safety considerations.
Conclusion
PsA has a diverse phenotype, and disease domains help us choose therapies most likely to be effective for each specific patient. When selecting a therapy, consider the patient’s worst disease domain and maximize coverage for other affected domains. Then, select the most effective bDMARD for those domains. Finally, consider each patient’s co-morbidities, preferences and safety context to narrow down options.

Samantha C. Shapiro, MD
Samantha C. Shapiro, MD, is a clinician educator who is passionate about the care and education of rheumatology patients. She writes for both medical and lay audiences and practices telerheumatology.
References
- Gossec L, Kerschbaumer A, Ferreira RJO, et al. EULAR recommendations for the management of psoriatic arthritis with pharmacological therapies: 2023 update. Ann Rheum Dis. 2024;83(6):706–719. doi:10.1136/ARD-2024-225531
- Coates LC, Soriano ER, Corp N, et al. Group for Research and Assessment of Psoriasis and Psoriatic Arthritis (GRAPPA): Updated treatment recommendations for psoriatic arthritis 2021. Nat Rev Rheumatol. 2022;18(8). doi:10.1038/s41584-022-00798-0
- Feld J, Chandran V, Haroon N, Inman R, Gladman D. Axial disease in psoriatic arthritis and ankylosing spondylitis: A critical comparison. Nat Rev Rheumatol. 2018;14(6). doi:10.1038/s41584-018-0006-8
- Husic R, Gretler J, Felber A, et al. Disparity between ultrasound and clinical findings in psoriatic arthritis. Ann Rheum Dis. 2014;73(8). doi:10.1136/annrheumdis-2012-203073
- Kaeley GS, Schett G, Conaghan PG, et al. Enthesitis in patients with psoriatic arthritis treated with secukinumab or adalimumab: A post hoc analysis of the EXCEED study. Rheumatology (United Kingdom). 2024;63(1). doi:10.1093/rheumatology/kead181
- Sbidian E, Chaimani A, Garcia-Doval I, et al. Systemic pharmacological treatments for chronic plaque psoriasis: a network meta‐analysis. Cochrane Database of Systematic Reviews. 2021;2021(4). doi:10.1002/14651858.CD011535.PUB4
- Singla S, Putman M, Liew J, Gordon K. Association between biological immunotherapy for psoriasis and time to incident inflammatory arthritis: A retrospective cohort study. Lancet Rheumatol. 2023;5(4). doi:10.1016/S2665-9913(23)00034-6