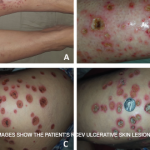
Because the medium vessels are barely within the reach of a punch biopsy, Dr. Seo noted that a full-excision biopsy would be necessary in many cases to establish a diagnosis. He showed photos of two patients that he said could very well be taken for cPAN, but neither one was.
“No matter how convinced you are of morphology, I can’t overestimate the value of a good biopsy when it comes to making these diagnoses,” he said.
The “slam dunk” finding on biopsy for this diagnosis is true evidence of blood vessel inflammation, but many other signs, including diffuse inflammation and occlusion of a vessel leading to neutrophilic activity, can be interpreted by a dermatopathologist as being consistent with vasculitis, even when other diagnoses should be entertained, he noted.
“Biopsy reports can be really hard to interpret, and I really suggest you not only read the headline, but you actually read the description of exactly what it is the pathologist saw before you agree with that diagnosis of vasculitis,” Dr. Seo said.
Treatment: Dapsone, azathioprine and, in severe cases, infliximab or cyclophosphamide, can play a role in treatment. Rest, elevation and compression stockings can help as well. Dr. Seo also emphasized the need for gentle debridement, because being too aggressive can cause the lesions to grow.
Urticarial Vasculitis
Urticarial vasculitis involves dermatalogic wheals that last longer than a day, with evidence of vasculitis on biopsy. Chronic urticaria can be differentiated from urticarial vasculitis by the absence of bruising or arthralgias, which are not commonly associated with this diagnosis.
Urticarial vasculitis comes in two forms: normocomplentemic type, which might resolve with dapsone or colchicine and is less likely to involve systemic features; and the hypocomplementemic type, which can be secondary to lupus (SLE), Sjögren’s syndrome and malignancies. Those patients with anti-C1Q antibodies are at a higher risk for hypocomplementemic urticarial vasculitis.
Treatment: The normocomplementemic type doesn’t generally require chronic therapy, although ongoing immunosuppression is sometimes needed, Dr. Seo said. Those with the hypocomplementemic type can be treated with azathioprine, sulfasalazine, rituximab or the IL-1 inhibitor canakinumab.
Thomas R. Collins is a freelance writer living in South Florida.