Recurrent cutaneous eosinophilic vasculitis (RCEV) is a rare autoimmune condition characterized histologically by necrotizing small vessel vasculitis of the skin and almost exclusive eosinophilic infiltration without any systemic involvement.1 Frequently, there is associated peripheral eosinophilia, and a prolonged course of glucocorticoids is required for treatment. To date, only a few RCEV cases have been reported.
Below, we describe a case of biopsy-proven RCEV with distinct, punched, ulcerative lesions and no evidence of peripheral eosinophilia; the patient remained glucocorticoid dependent despite multiple steroid-sparing agents. We also present a review of the literature and discuss the clinical features, histopathological features and differential diagnosis for RCEV.
The Case
A 75-year-old Caucasian woman presented with a two-year history of recurrent skin eruptions over her legs, buttocks and arms, sparing the trunk. These lesions started as intensely pruritic urticarial lesions that developed into vesicles and pustules and then progressed to eczematous punched ulcers within two to three weeks (see Figures 1A–D, above right). Treatment with antihistamines and antibiotics proved ineffective.
A systems review was otherwise unremarkable. The patient’s past medical history revealed allergic rhinitis that had been quiescent for several years and no history of asthma. Current medications did not include any agents likely to cause a drug eruption.
The complete blood count was unremarkable. Importantly, the patient never had peripheral eosinophilia on initial presentation or throughout the two years of her disease. Tests for anti-nuclear antibodies, anti-extractable nuclear antigen antibodies, anti-neutrophil cytoplasmic antibodies, rheumatoid factor, anti-cyclic citrullinated peptide antibodies, double-stranded DNA antibodies, serum cryoglobulins and serology for HIV, hepatitis B and hepatitis C were all negative on several occasions. Complement levels were normal. C-reactive protein was never elevated unless the patient had developed infections.
Two bone marrow biopsies to determine a hematological cause of eosinophilic infiltration were unremarkable. The patient also underwent eight skin biopsies, most of which demonstrated eosinophilic infiltration, ulceration and superficial and deep perivascular inflammation with vascular damage (see Figure 2A). Two biopsies showed cutaneous small vessel vasculitis with fibrinoid necrosis of vessel walls and surrounding nuclear debris (see Figures 2B & 2C).
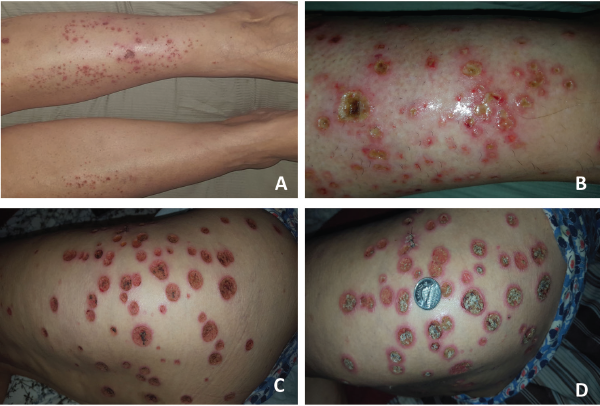
Figure 1. These images show the patient’s RCEV ulcerative skin lesions over two weeks, including image A, which shows an intensely pruritic urticarial rash on her lower legs bilaterally; B, which shows progressive worsening and the development of vesicles and pustules with proteinaceous exudates; C, which shows the formation of eczematous, punched ulcers over her buttocks and thighs; and D, an enlarging ulcer base with crusting (and a Canadian quarter placed to demonstrate ulcer size).
Diagnosis
The patient was diagnosed with recurrent cutaneous eosinophilic vasculitis.
We did an extensive search for other organ involvement, which included a normal echocardiogram, non-specific minimal groundglass opacity on chest computed tomography and a mild obstructive pattern on pulmonary function testing in keeping with chronic obstructive pulmonary disease. The patient also suffered long-standing microscopic hematuria without an active sediment or renal dysfunction, which was attributed to bladder diverticula on cystoscopy and recurrent urinary tract infections.
The patient’s lesions were highly responsive to prednisone, but her skin lesions recurred whenever the prednisone was tapered below 10 mg daily. After two years of glucocorticoid therapy, she developed multiple side effects, including weight gain, osteoporosis and hypomania. She was initially treated with azathioprine, but developed significant nausea and diarrhea, so she was transitioned to 25 mg of methotrexate subcutaneously weekly and 400 mg of hydroxychloroquine daily, which were ineffective in controlling the lesions. Subsequently, tacrolimus was initiated, but she developed acute renal injury, which resolved upon withdrawing tacrolimus. Further therapy escalation to more potent immunosuppression, such as mycophenolate or cyclophosphamide, was limited due to recurrent urinary tract infections with resistant organisms.
She was on 10 mg of prednisone daily and methotrexate when she succumbed to pneumosepsis and respiratory failure.