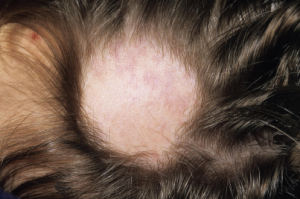
Hair loss is commonly seen in lupus patients, but not all alopecia types are the same.
Dr P. Marazzi/Science Source
SAN DIEGO—Rheumatologists who treat lupus patients gleaned tips on diagnosis and management of renal disease, painful neuropathies and alopecia at a “Curbside Consults” session held Nov. 6 at the ACR/ARHP Annual Meeting in San Diego.
Membranous Lupus Nephritis
Patients with refractory membranous lupus nephritis (MLN), or Class V lupus nephritis, face “significant morbidity, most of which is related to nephrotic syndrome and hypo-albuminemia,” said Ellen M. Ginzler, MD, MPH, distinguished teaching professor of medicine and chief of rheumatology at SUNY Downstate Medical Center in Brooklyn, N.Y. About 20% of lupus nephritis patients have MLN, and 10% may progress to end-stage renal disease after 10 years.1
“So this is not a trivial problem. It’s important to think about possible consequences when you choose initial treatment,” including women who wish to become pregnant later, she said. Current ACR guidelines recommend pulse prednisone with a range of 0.5 to 1 mg/kg a day and immunosuppressant therapy, but “the question is which immunosuppressant drug to use?”2 Both the ACR and EULAR guidelines suggest mycophenolate mofetil (MMF), but intravenous cyclophosphamide is another option.3 She shared a case of a nulliparous, 32-year-old woman with MLN who started on 30 mg of prednisone and 3 g of MMF daily, and Dr. Ginzler suggested that African American and Afro-Caribbean patients may do better on the higher range of the recommended dose.
Although her patient’s blood pressure was normal, Dr. Ginzler also prescribed losartan, an angiotensin receptor blocker (ARB). ARBs and angiotensin-converting enzyme inhibitors “may lower proteinuria, but give you a false sense of security, because what they do is decrease renal blood flow, not really affecting the glomerular pathology” in MLN patients, she said. When her patient later wanted to conceive, she switched from MMF to azathioprine, although it can elevate risk of renal flare in some patients, said Dr. Ginzler.
“Unfortunately, my patient was one of them, and eight months later, she had a flare, and again had hypo-albuminemia and significant nephrotic syndrome,” she said. Renal biopsy confirmed that she still had pure MLN, so she restarted induction therapy with a slightly higher prednisone dose. She redeveloped leg edema, still had proteinuria, and was later confirmed to have renal vein thrombosis. She started anticoagulation therapy, and then Dr. Ginzler and her colleagues chose to also start cyclosporin, a calcineurin inhibitor, based on current guidelines. Trials of calcineurin inhibitors are few, small, mainly anecdotal and do not focus on patients with pure MLN, she said. One meta-analysis focused on pure MLN patients suggests rituximab is another option, with 40% of patients achieving complete and 27% achieving partial response.4

