The Interesting Glitch
“Physicians find lupus so difficult to a great extent because the disease manifests differently in different individuals,” Dr. Silverman says. “Add in the variability of disease activity—remission, exacerbations and progression—and you have a perfect storm of clinical challenges.
“I reflect deeply on each case, asking myself, ‘Who are these patients, and how are they affected by the disease?’ We have data with which we can do a sophisticated computational analysis of the microbiome … and when doing so I always consider that set of twins from many years ago. What would they look like? Would the microbiome in a healthy (non-active disease) patient be different than one in someone with active lupus? Some of the patients in our study were very ill, while others were feeling well [i.e., were not taking medication and had no detectable disease activity].
“I knew that what we were undertaking was not going to be a simple analysis where we would compare controls to people with disease,” Dr. Silverman explains. “I decided that we needed three groups: healthy patients, those with active lupus and those with inactive lupus.”
‘We found the microbiome of patients with SLE also showed decreased species richness diversity, with the most significant reductions in taxonomic complexity in patients with high disease activity.’ —Dr. Silverman
Pattern Identification
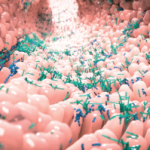
Those were the first threads of an effort that resulted in the identification of a pattern in which the presence of a single type of bacteria was expanded in the intestines of lupus patients. The more of the bacteria that was present, the sicker the patients were.
“We found the microbiome of patients with SLE also showed decreased species richness diversity, with the most significant reductions in taxonomic complexity in patients with high disease activity [as measured by the SLE disease activity index; SLEDAI],” Dr. Silverman says.
“Particularly interesting was the finding that patients with SLE had a fivefold greater representation of Ruminococcus gnavus [RG] in their guts. While RG is not necessarily bad or uncommon, we found that if one particular strain exists in a lupus patient then that person will become sick,” he explains.
“We found that some strains produce a molecule called a lipoglycan. While in some individuals the lipoglycan could normally be innocuous and sealed in the intestinal tract, we believe that in these cases, it is thrown off in the local intestines and released because of a leaky gut. We found that not only do lupus patients have more of this bacteria [RG], but that the patients exhibit a strong antibody response to this type of molecule in one species. So in patients who develop kidney disease, some part of the bowel is like a screen door … things are getting let out, which may be driving the autoantibody response that leads to nephritis.
“At this point,” Dr. Silverman says, “we have been able to develop enough data along with a testable hypothesis that perhaps lupus patients have too much of this one bad strain of bacteria. Going forward, we should be developing early testing for this bacterium, its lipoglycan and antibodies to the lipoglycan. The next goal would be to eliminate the released lipoglycan.”
Commenting on the research process, Dr. Silverman notes, “At certain points I was a bit discouraged because all of the patients were so different from one another. Some were experiencing joint issues while others had rashes—and the rashes often differed from patient to patient. I thought, ‘Is lupus really one disease?’
“It looked like so many different conditions that I was reminded of the … story where seven blind men each touched different parts of an elephant, and each thought it was something different,” he says. “It was tenacity that kept us going. Using the SLEDAI scale was a bit of a risk, because it is rather simple and not meant to be used for the microbiome. We borrowed tools during this exploratory process and luckily, they turned out to be relatively useful. That both active and inactive lupus patients could be involved in one study and get such clarity was unexpected and very promising.”