The disease is seen in the kidney between 45% and 85% of the time, with renal insufficiency seen about 30% of the time in adults, but in children, kidney involvement is much rarer.
Adult vs. Pediatric Presentation
There are major differences between the child and the adult versions of the disease. In adults, renal issues are worse; the disease tends to be relapsing-remitting rather than self-limiting, as in children; there tend to be more complications; and the response to treatment is largely unknown because almost all of the studies have been done in pediatrics.
Also in adults, there is no seasonal pattern, while in children it tends to be seen in fall and winter; there are multiple causes in adults, while in children it tends to follow an infection. Children tend to fare better, with a complete recovery rate of about 80%, compared with 40% in adults, and chronic renal failure is seen in 2% of children, compared with about 10% of adults.
Testing
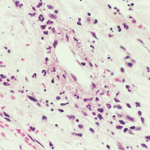
A clinical question surrounding IgA vasculitis is whether it’s helpful to do direct immunofluorescence (DIF) along with a biopsy. One study, now fairly dated and not replicated, found that DIF had a low predictive value in cases with a low clinical suspicion.1
“That’s just one thing to think [about],” Dr. Villa-Forte said. “I think at this stage of the understanding of this disease that we still need these studies in all patients.”
The ideal is to have a fitting clinical presentation, along with a tissue biopsy showing leukocytoclastic vasculitis with IgA deposits.
“If you have all this, then you can be sure about the diagnosis, but if you don’t, there’s always the possibility that it’s not the right diagnosis,” she said.
Pathophysiology
The disease is brought about by the deposits of polymers involving molecules of IgA1 that are galactose deficient, a status that appears as though it might be altered by genetics.
“It’s a high molecular polymer that is very heavy and deposits more easily,” Dr. Villa-Forte said.
A key question is what happens from the time of the deposit to when disease occurs.
“That’s what we don’t know,” said Dr. Villa‑Forte.
Factors that could play an important role include CD89, the human IgA Fc receptor, and CD71, a receptor that’s in the monocyte where the aggregate links.
Treatment
“That might be the hope for two things: diagnostic tests and treatment,” Dr. Villa‑Forte said. “We do not have good treatment or treatment that has been proved to make any difference in nephritis.”