Background
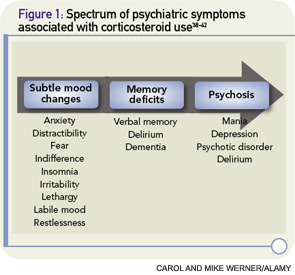
Corticosteroids are used to treat inflammatory manifestations of many rheumatologic conditions. Doses necessary to control disease are frequently high (e.g., 1 mg/kg or greater), and therapy may be maintained for prolonged periods of weeks to months. In this setting, one out of every two to three patients prescribed steroids may develop psychiatric symptoms including psychosis, mania, delirium, and depression. The most common symptoms reported with corticosteroid therapy are hypomania, mania, and psychosis.1