The primary risk factor for the development of corticosteroid-induced psychosis is a high dose of corticosteroids, with a sharp increase in risk among patients taking 40 mg of prednisone or its equivalent daily.4,9 Corticosteroid dosage, however, has not been correlated with onset, severity, type of reaction, or duration of psychiatric symptoms.3,9 Corticosteroid-induced psychosis is more common in women than in men. A history of psychiatric disorders or previous corticosteroid-induced psychosis is not predictive of future episodes.3
Treatment of Corticosteroid-Induced Psychosis
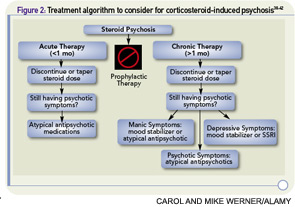
Whenever possible, tapering corticosteroids is recommended as a first step to manage corticosteroid-induced psychosis. Decreasing to the lowest dose possible, ideally less than 40 mg daily, or tapering and discontinuing steroids may be sufficient to improve psychiatric symptoms without requiring additional medications. In severe cases of affective instability or psychosis or if steroids cannot be tapered or discontinued, it may be necessary to employ off-label psychopharmacologic treatment. There is some evidence from open-label trials and case reports to support a role for antipsychotics and mood stabilizers. Studies with anticonvulsants have not supported their use.10–22
Although there is evidence to support mood stabilizers such as valproic acid, carbamazepine, and lithium in the treatment of steroid psychosis, the use of these medications can be complicated in medically ill patients.3 Of these three medications, valproic acid would be the most reasonable choice; however, this has been associated with pancreatitis and thrombocytopenia, and monitoring of liver enzymes is recommended. Because of possible drug interactions, carbamazepine, a potent inducer of cytochrome P450 isoenzyme activity, can be complicated to use in patients taking prednisone and other medications. Carbamazepine also requires monitoring for agranulocytosis and the possible development of the syndrome of inappropriate antidiuretic hormone section (SIADH).
Because many patients prescribed corticosteroids have rheumatological illnesses that affect renal function, lithium may be difficult to use safely in this patient population. Lithium has a narrow therapeutic index, is metabolized through the kidneys, and is not safe for use with angiotensin converting enzyme (ACE) inhibitors, nonsteroidal antiinflammatory drugs (NSAIDs), or diuretics. Although antipsychotics also have risks, including increased risk for the development of the metabolic syndrome and QTc prolongation, using these medications at the lowest effective dose for the minimum necessary duration can be an effective strategy to treat steroid psychosis.
Antipsychotics
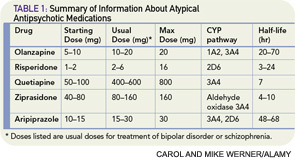
There is general support for the use of low-dose atypical antipsychotic agents when symptoms are severe or when tapering steroids is not feasible; the specific drug or dose recommendation is informed by personal preference of the provider as well as by limited evidence. In a five-week, open-label trial of 12 outpatients experiencing manic or mixed symptoms associated with corticosteroid use, olanzapine was associated with significant reductions in psychiatric symptoms on the Young Mania Rating Scale, the Hamilton Rating Scale for Depression, and the Brief Psychiatric Rating Scale.16 There were no statistically significant differences in weight or blood glucose, although it is important to note that this was a small trial of short duration and, on average, patients gained five pounds in five weeks on this medication. Case reports of olanzapine indicate that starting at a low dose (e.g., 2.5 mg) and titrating up to a moderate dose (e.g., 10–15 mg) daily can be effective in alleviating symptoms.15–17