There are four case reports describing a benefit from risperidone, with doses ranging from 1 to 4 mg daily, in adults and children with a variety of psychiatric symptoms, including hypomania, hallucinations, and delusions associated with corticosteroid therapy.18–21 In these patients, symptoms improved within days to weeks. One case report described the successful use of quetiapine 25 mg daily with a 12.5-mg as-needed dose for the treatment of corticosteroid-induced mania.22 No case reports exist for ziprasidone or aripiprazole. Table 1 (p. 41) contains information about dosing, metabolism, and half-life of the atypical antipsychotics. Of the typical (first generation) antipsychotics, there are case reports for the use of low-dose haloperidol (2–5 mg daily)23 and chlorpromazine (150 mg daily).24
Monitoring Considerations
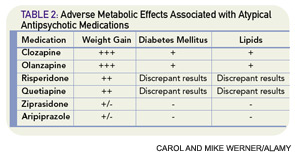
The use of atypical antipsychotics has been associated with the development of the metabolic syndrome (see Table 2, p. 41). The American Psychiatric Association, American Diabetic Association, American Association of Clinical Endocrinologists, and American Association for the Study of Obesity coauthored guidelines for suggested monitoring of patients prescribed these agents.25 Before starting atypical antipsychotics, baseline personal and family history along with body mass index, waist circumference, blood pressure, fasting plasma glucose, and fasting lipid profile should be obtained. Weight should be monitored monthly for the first three months and then quarterly, and blood pressure and fasting glucose should be rechecked (and treated, if abnormal and unable to taper off the antipsychotic medication) after three months and then annually while prescribed the medication.25
Atypical antipsychotics are also associated with various side effects, and monitoring for development of extrapyramidal side effects is recommended (see Table 3, above). Given the adverse side-effect profile and off-label use, these medications should be used at the lowest effective dose for the shortest effective duration. Though there are no clear monitoring recommendations, all antipsychotics can prolong the QTc interval.
Mood Stabilizers
A retrospective cohort study examined records of patients diagnosed with multiple sclerosis or retrobulbar neuritis who were treated with corticotrophin and assessed their outcomes based on whether or not they received prophylactic lithium therapy.13 Psychiatric symptoms developed in 38% of patients treated with lithium at doses to maintain serum levels between 0.8 and 1.2 mEq/L compared with 62% of controls, and none of the lithium-treated patients developed frankly psychotic symptoms. There are also case reports describing the use of lithium, valproic acid, and carbamazepine as prophylaxis or as treatment of corticosteroid-induced psychosis.26–33 Unfortunately, the lack of controls makes interpretation of these reports difficult, particularly because previous history of corticosteroid-induced psychosis is not reliably predictive of future development of the same symptoms.3