Research has shown that anticonvulsants are teratogens and pose a risk for fetal malformations. Meadow was the first to note a possible link between congenital abnormalities and maternal use of anticonvulsive drug in 1968.1 In 1974, Barr et al noted hypoplasia and irregular ossification of the digital distal phalanges with nail dystrophy in children born to epileptic mothers who were taking anticonvulsive medications.2
In 1975, Hanson and Smith identified special clusters of anomalies, including craniofacial features, microcephalus, mental retardation and hypoplasia of the distal phalanges in the offspring of women taking phenytoin, and they proposed calling these specific phenytoin-related anomalies fetal hydantoin syndrome (see Table 1).3,4
Since then, several authors have substantiated this association, especially with diphenylhydantoin (phenytoin). Most of the articles and case reports concerning this problem have been limited to pediatrics and orthopedics. Hand abnormalities have been reported as consistent features of this syndrome and act as a genetic marker indicating more serious teratogenic effects.5
In our case, a patient presented with distal limb deformities at the age of 19 in an adult rheumatology clinic. This case is a great way to bring these congenital musculoskeletal deformities and more serious underlying abnormalities to the attention of both pediatric and adult rheumatologists. Also, knowledge and awareness will offer cost savings related to unnecessary testing and referrals.
Case Report
A 19-year-old young man presents with his father in the adult rheumatology clinic for evaluation of “nodes on his knuckles.” He was referred by his primary care physician due to deformities of his hands and feet. He denies any symptoms, and a complete review of his systems is negative.
His father mentions that his son has a history of cardiac murmur; however, the patient’s previous complete cardiac evaluation, including echocardiogram, is unremarkable. He is otherwise healthy and has no other past medical history.
He is adopted and is of Mexican Cuban heritage. His biological mother had a history of epilepsy. He does not smoke or drink alcohol. He does not take any medication on a regular basis.
His physical exam is significant for a grade II systolic murmur.
His musculoskeletal exam shows tapering of his fingers distally, with hypoplastic distal phalanges and fingernails (see Figure 1). He also has flexion deformities of the distal interphalangeal joints and slight extension of his proximal interphalangeal joints, more pronounced over the fourth and fifth digits (see Figures 2 and 3). His distal interphalangeal flexion deformities are reversible on exam (Jaccoud’s arthropathy). His thumbs are thinner than normal (see Figure 4).
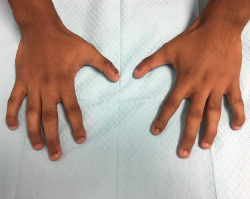
Figure 1. Bilaterally, the hands demonstrate hypoplasia of distal phalanges, hypoplastic nails and flexion of distal interphalangeal joints.
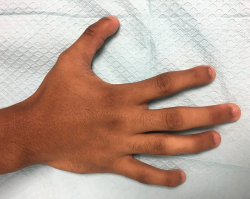
Figure 2. This image of the right hand gives us a closer view of the fourth and fifth digits; however, the mild extension of the proximal interphalangeal joints is not well visualized in the picture.

Figure 3. This image of the left hand gives us a closer view of the fourth and fifth digits; however, the mild extension of the proximal interphalangeal joints is not well visualized in the picture.

Figure 4. Bilaterally, the thumbs have a thinner-than-normal appearance, with hypoplastic nails.
His feet show hypoplastic distal phalanges and toenails, bilaterally (see Figure 5). He is also found to have flexion deformities of distal interphalangeal joints in his feet (see Figure 6).
X-rays performed in the office reveal hypoplasia of the distal phalanges in his hands (see Figures 7 and 8) and feet (see Figures 9 and 10).
His comprehensive metabolic panel and vitamin D and parathyroid hormone levels are all normal. A review of his transthoracic echocardiogram report from four years earlier is normal, except for trace tricuspid valve regurgitation.
His hand and foot abnormalities are thought to be congenital malformations, and they are also suggestive of fetal hydantoin syndrome. After reviewing many studies supporting this diagnosis and having detailed discussions with the patient and his father, we did not pursue any further workup, including genetic testing. The patient did not have evidence suggestive of any other underlying abnormalities.

Figure 5. Bilaterally, the feet have hypoplasia of the distal phalange

Figure 6. Hypoplastic nails and flexion of the distal phalangeal joints.
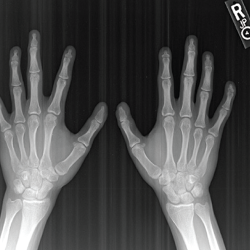
Figure 7. An X-ray of both hands—antero-posterior view—shows hypoplasia of the distal phalanges, which is more pronounced over the second and fifth digits.

Figure 8. An X-ray of both hands—oblique view—shows hypoplasia of the distal phalanges.

Figure 9. An X-ray of both feet—antero-posterior view—shows hypoplasia of the distal phalanges and subluxation of the distal interphalangeal joints.

Figure 10. An X-ray of both feet—oblique view—shows hypoplasia of the distal phalanges.
Discussion
This case report illustrates the musculoskeletal anomalies seen in fetal hydantoin syndrome. Hypoplastic distal phalanges and fingernails are common features. In this case, the patient did not represent the full picture of the syndrome.
The full syndrome can include hypoplastic distal phalanges with small fingernails, a digital-type thumb, abnormal palmar creases, increased frequency of low arch, digital dermal ridge patterns and hip dislocation. Our patient had only hypoplastic distal phalanges, small fingernails and a thinner-than-normal thumb, described as a digital-type thumb.
A case was reported in the orthopedic literature showing hip dysplasia discovered in a 23-year-old male with hypoplasia of fingernails and distal tapering of fingers due to fetal hydantoin syndrome.6 However, the same patient also had mild mental retardation, which fortunately was not the case in our patient.
Fetal hydantoin syndrome affects males and females in equal numbers. The exact incidence and prevalence of the disorder are unknown. Various studies have suggested an approximate incident rate of 5–10% of fetal hydantoin syndrome in infants exposed to phenytoin in utero.
No diagnostic testing can identify fetal hydantoin syndrome. A diagnosis is made clinically based upon identification of characteristic symptoms in an affected infant in conjunction with a history of phenytoin exposure during gestation.
It has been also noted that the majority of infants born to women who take phenytoin during pregnancy will not develop fetal hydantoin syndrome. It is not clear whether the adverse effects of phenytoin during fetal development are due to the drug itself or if they are caused by one of phenytoin’s metabolites. The potential role of other factors, such as genetic influences that affect phenytoin metabolism or additional environmental factors (e.g., smoking), remains unclear. There have been reports in the medical literature that women with mutations in the methylenetetrahydrofolate reductase (MTHFR) gene are at an increased risk of having an infant with fetal hydantoin syndrome.
Evidence is accumulating from clinical reports and animal experiments to support the notion that mild distal digital hypoplasia is a relatively specific marker for in utero exposure to the drug. More severe digital involvement has also been identified, although to a lesser extent, in animal experiments and in only a few humans exposed to the drug in utero.
Apart from digital involvement, an association between in utero exposure to diphenyl-hydantoin and more proximal (carpal metacarpal) anomalies has yet not been reported.7 The frequent finding of low arch dermal ridge patterning on affected fingertips indicates that the fetal fingertip pads were hypoplastic by 15–20 weeks of fetal life, the age when dermal ridge development and patterning is established. The severity of defects varies from the more common mild hypoplasia of nails and distal phalanges, as in our patient, to the more unusual gross deficiency of whole digits, as reported in some cases.8
Many syndromes noted in the pediatric literature include nail hypoplasia or dysplasia. The pattern of multiple abnormalities seen in each of these entities usually makes a specific diagnosis possible. One entity that can be confused with the fetal hydantoin syndrome is the Coffin-Siris syndrome. This syndrome has several similarities to fetal hydantoin syndrome, including hypoplastic fingernails and toenails, especially of the fifth digits; however, Coffin-Siris patients are more severely retarded and often have joint laxity and dislocation of the radial head.2
Treatment
Treatment for the hypoplastic distal phalanges and nails is rarely indicated. Their appearance may improve with time, especially with regard to the nails. However, it is important to recognize this congenital hand defect in children of epileptic women using hydantoin drugs, because this defect serves as a skeletal marker that may point the physician toward other, more severe, congenital abnormalities.
 Reshma Khan, MD, is a rheumatologist at the Family Arthritis Center in Jupiter, Fla.
Reshma Khan, MD, is a rheumatologist at the Family Arthritis Center in Jupiter, Fla.
 Andrew Evans, DO, is the chief resident for internal medicine at Wellington (Fla.) Regional Medical Center.
Andrew Evans, DO, is the chief resident for internal medicine at Wellington (Fla.) Regional Medical Center.
Acknowledgment
To the patient who gave us the trust to manage his care and permission to report this case.
References
- Meadow SR. Anticonvulsant drugs and congenital abnormalities. Lancet. 1968 Dec 14;2(7581):1296.
- Silver L. Hand abnormalities in the fetal hydantoin syndrome. J Hand Surg Am. 1981;6(3):262–265.
- Hanson JW. Teratogen update: Fetal hydantoin effects. Teratology. 1986 Jan;33:349–353.
- Singh A, Bhatia HP, Mohan A, Sharma N. Fetal hydantoin syndrome: A case report. J Indian Soc Pedod Prev Dent. 2016 Jan–Mar;34(1):92–95.
- Loughnan P, Vance J, Gold H. Phenytoin teratogenicity in man. Lancet. 1973 Jan 13;301(7794):70–72.
- Trousdale RT. Fetal hydantoin syndrome: An usual cause of hip dysplasia. Orthopedics. 1998 Feb;21(2):210–212.
- Sabry MA, Farag TI. Hand anomalies in fetal-hydantoin syndrome: From nail/phalangeal hypoplasia to unilateral acheiria. Am J Med Genet. 1996 Apr 24;62:410–412.
- Smith DW. Distal limb hypoplasia in the fetal hydantoin syndrome. Birth Defects Orig Artic Ser. 1977;13(1):355–359.