ATLANTA—Diagnosing and treating granulomatosis with polyangiitis (GPA) and relapsing polychondritis (RP), two diseases associated with chondritis, often require patience, thoroughness and, as Philip Seo, MD, MHS, said during a session at the 2019 ACR/ARP Annual Meeting in November, time. In one case he presented during the session, perhaps a full year.
Dr. Seo is director of the Johns Hopkins Vasculitis Center, Baltimore, and the physician editor of The Rheumatologist. His talk was titled, Are Your Ears Burning? Cartilaginous Inflammation in Relapsing Polychondritis & Limited GPA. The “ears burning” part of the title illustrated part of the diagnostic dilemma: not only are GPA and RP rare, but they share symptoms of many other diseases, including manifestations that can affect the appearance and function of the ear.
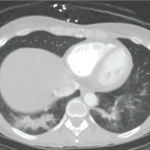
RP is a chronic condition of cartilage that can appear as recurrent episodes of inflammation throughout the body. In addition to the ears, other sites affected are the nose, joints, spine and trachea. GPA (formerly known as Wegener’s granulomatosis) is associated with granulomas and vasculitis.
Dr. Seo said that in his experience, diseases that can be associated with chondritis can present similarly to include Behçet’s disease (MAGIC syndrome), which can feature mouth and genital ulcerations with inflamed cartilage. Other possibilities include retroperitoneal fibrosis, and diseases affecting the gastrointestinal, cutaneous, endocrine and hematologic systems.
Rheumatoid arthritis and spondyloarthritis are rarely associated with a finding of chondritis, according to Dr. Seo. “To me, the difference is that patients with GPA and RP generally won’t have erosions on their X-rays,” he said. Systemic lupus erythematosus is also on the list of diseases that can be associated—rarely—with chondritis, as is familial Mediterranean fever.
Being thorough to get the diagnosis right is important, because getting it wrong can ultimately be life threatening. “My philosophy is that when you’re treating a patient, you try to treat the underlying diagnosis first, rather than trying to treat the chondritis as a separate issue. If you can get the underlying disease under control, often the chondral manifestations will also go away.”
The Ears Have It
The ear is the most common site associated with chondritis and includes manifestations resembling a cauliflower ear. “This is not the only manifestation you may see,” said Dr. Seo. “In a patient with bad GPA or RP, there may be a collapse of the ear canal itself, resulting in hearing loss, because the sound can’t get through to the ear drum.”