In March 2020, an elderly married couple living on Long Island, N.Y., presented to our emergency department with symptoms suspicious for COVID-19 infection.
The wife, a-76-year-old woman, presented with complaints of subjective fevers, minimal dry cough and headaches of one-week duration. She denied having any chills, rhinorrhea, diarrhea, abdominal pain or shortness of breath. Two days earlier, she had presented with similar symptoms, but was discharged home.
Her past medical history was significant for seronegative rheumatoid arthritis, diagnosed in 2006; hypertension; coronary artery disease; hyperlipidemia; and gastroesophageal reflux. She had previously had hand surgery and cataract surgery. She had been on etanercept 50 mg weekly, methotrexate 10 mg weekly for more than 10 years, olmesartan, metoprolol, omeprazole and nortriptyline. She had no recent travel history.
On admission, she had a temperature of 37.6º C, with a pulse of 88 beats/minute, a respiratory rate of 24 breaths/minute and a blood pressure of 184/74 mmHg. Her body mass index (BMI) was 28.1 kg/m2. Her lungs were clear to auscultation and no murmur was appreciated; there were no signs of synovitis or joint deformities; the remainder of her physical exam was reported to be without abnormalities.
Abnormal laboratories included sodium 125 mmol/L (reference range [RR]: 135–146), chloride 83 mmol/L (RR: 96–107), glucose 136 mg/DL (RR: 70–99), alanine transaminase 35 UI/L (RR: 0–33), aspartate transaminase 51 UI/L (RR: 0–32), white blood cell count of 4,550 cells/mm3 (RR: 4,800–10,800), with a lymphocyte count of 250 cells/mm3 (RR: 900–4,800) and a procalcitonin of 0.05 ng/mL (RR: <0.10). Her C-reactive protein (CRP) was 1.2 mg/dL (RR: 0–0.5) on day 3 of hospitalization, and her erythrocyte sedimentation rate (ESR) (RR: 0–30 mm/h) and D-dimer were within normal limits. Her interleukin 6 (IL-6) was 12.8 pg/mL (RR: <14.8). She had a negative QuantiFERON TB test (mitogen 10 IU/mL).
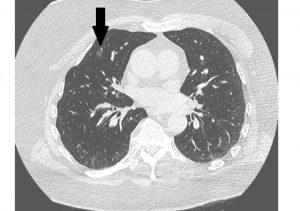
Her chest X-ray and chest computed tomography (CT) were clear, without any infiltrates. Other than an elevated temperature of 38.1° C on hospital day 3, her symptoms quickly abated.
A nasopharyngeal swab obtained on admission was positive for SARS-CoV-2 by polymerase chain reaction (PCR) (Viracor Eurofins, Lee’s Summit, Mo.). She did not require any supplemental oxygen, hydroxychloroquine, azithromycin, nor any antiviral agents; she did receive acetaminophen, but did not receive methotrexate or etanercept during the hospitalization.
Her husband, a 78-year-old man, presented to the emergency department complaining of high fevers (38.9º C) and severe dry cough for the previous 24 hours, along with fatigue, myalgias, shortness of breath, frontal headaches and lightheadedness.