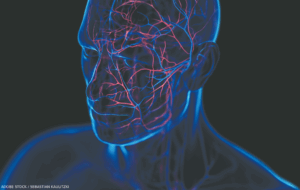
 WASHINGTON, D.C.—Multiple game-changing studies on the assessment and management of systemic vasculitis were presented at ACR Convergence 2024. Here, we highlight important points from seven of these studies. They focus on new treatment strategies for a range of diseases, including giant cell arteritis (GCA), anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis and IgG4-related disease (immunoglobulin G4-RD).
WASHINGTON, D.C.—Multiple game-changing studies on the assessment and management of systemic vasculitis were presented at ACR Convergence 2024. Here, we highlight important points from seven of these studies. They focus on new treatment strategies for a range of diseases, including giant cell arteritis (GCA), anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis and IgG4-related disease (immunoglobulin G4-RD).
1. Upadacitinib for GCA
Abstracts 0770 & 1695: Merkel et al.1,2
Upadacitinib (UPA) is an oral Janus kinase (JAK) inhibitor that was recently approved by the U.S. Food & Drug Administration (FDA) for the treatment of giant cell arteritis, based on the data presented in these abstracts. It had previously been approved by the FDA for several other indications, including rheumatoid arthritis, ankylosing spondylitis, non-radiographic axial spondyloarthritis and psoriatic arthritis.
SELECT-GCA is a double-blind trial that randomized 428 patients with new (70%) or relapsing (30%) GCA to receive treatment with upadacitinib (UPA; 7.5 mg or 15 mg daily with a 26-week glucocorticoid taper) or placebo with a 52-week glucocorticoid taper.3
Patients treated with the higher dose of UPA were significantly more likely to achieve sustained remission (defined as the absence of disease activity from week 12 through week 52) and adherence to the glucocorticoid taper than patients treated with placebo (46% vs. 29%, P=0.002). They were also more likely to have a decrease in flare rate, fatigue and cumulative glucocorticoid exposure. Patients treated with the lower dose of UPA did not achieve any of these end points. This was true across subgroups based on age, sex, new-onset disease and history of polymyalgia rheumatica.
Patients treated with 15 mg of UPA had higher rates of herpes zoster, lymphopenia, anemia and nonmelanoma skin cancer (NMSC), but did not have higher rates of venous thrombotic events, non-NMSC malignancies or major adverse cardiovascular events (MACE).
When I was in training, I was taught that GCA could only be treated with glucocorticoids. Clearly, this is no longer the case. Tocilizumab, the first biologic approved by the FDA for the treatment of GCA, has dramatically changed outcomes for many patients afflicted with this common cause of systemic vasculitis.4 However, many patients are reluctant to use tocilizumab because of contraindications, payer issues or a hesitancy to use an injectable drug. For patients in all of these groups, upadacitinib, an orally administered JAK inhibitor, may represent a welcome option.
Upadacitinib, like all JAK inhibitors, has a boxed warning indicating an association with MACE (e.g., cardiovascular death, myocardial infarction, stroke), venous thrombotic events and malignancies; some studies indicate these risks may be higher among older patients.5 It is, therefore, reassuring that SELECT-GCA did not detect an association between UPA and any of these adverse events. However, longer-term follow-up will be required before we can completely dismiss these concerns.