On admission, he complained of double vision that progressed to complete visual loss OS during the week prior to admission. His sinus symptoms persisted and he reported frequent nasal discharge that was green and occasionally brown and bloody. He noted a persistent feeling of numbness on his left cheek and forehead. He reported severe fatigue and an 80-pound weight loss over the prior four months. He continued to have lower urinary tract symptoms with intermittent gross hematuria, which he attributed to self-catheterization. He denied fevers, chills, night sweats, hearing loss, respiratory symptoms, abdominal pain, changes in bowel habits, joint pain, numbness, or weakness of his extremities.
His medications included doxycycline, glyburide, timolol, and travoprost eye drops. He had no allergies or family history of rheumatologic disease. He previously worked as a realtor but had to stop working due to his illness. He lived alone without pets. He had traveled to Bermuda during the previous year and denied known exposure to tuberculosis. He smoked two packs per day for 30 years but quit 12 years prior.
On exam, he appeared chronically ill with temporal wasting bilaterally. He had proptosis of the left eye with left nasal bridge and periorbital edema. He was unable to open the left eye on his own. With assistance, it was noted that his left eye was deviated to the left and he had limited ocular movement in all directions. The sclera were clear. Nasal examination demonstrated mild congestion anteriorly without perforation. Neurological exam revealed loss of sensation in the V1–V2 distribution of the trigeminal nerve. His lungs were clear. There was no evidence of synovitis or skin lesions.
Laboratory workup revealed a white blood cell (WBC) count of 11,900 (ref 4.8–10.8 x 1000) with neutrophil predominance, creatinine 0.87mg/dL (ref 0.8–1.3 mg/dL), erythrocyte sedimentation rate (ESR) 92 mm/hr (ref <11 mm/hr), and C-reactive protein (CRP) 91.1mg/L (ref <8 mg/L). Antinuclear antibody, ANCA, human immunodeficiency virus, angiotensin converting enzyme, purine protein derivative (PPD), 1-3 B-glucan, and galacatomannan testing was negative. Urinalysis revealed greater than 100 red blood cells (RBCs) and greater than 100 white blood cells (WBCs) per high power field. Review of the sediment did not demonstrate any dysmorphic RBCs or RBC casts. Urine cultures grew >100,000 CFU/ml of C. albicans. Blood cultures were negative.
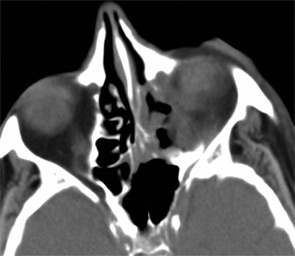
Imaging of the orbit demonstrated destruction involving the left lateral nasal wall, floor of the orbit, middle turbinate, roof of the nasopharynx, and the sphenoid sinus with abnormal soft tissue density along the left medial orbital wall and orbital floor with extension through several skull base foramina (see Figure 1). A chest CT demonstrated a right-middle lobe cavitary lesion measuring 2 cm by 2 cm with a small satellite lesion (see Figure 2). An abdominal CT demonstrated a locally invasive process involving the prostate gland, bladder, and seminal vesicles, as well as a 2.7cm by 2.1 cm renal mass (see Figure 3).