ANCA testing, when performed using enzyme-linked immunosorbent assay (ELISA) and immunoflorescence testing, is up to 96% sensitive in systemic disease, but only up to 83% sensitive in localized disease.1,2 While RB had systemic disease, including lung and genitourinary (GU) involvement, he was in the small minority of patients that is ANCA negative despite repeated testing.
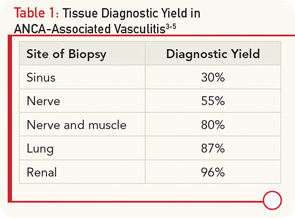
In the absence of ANCA positivity, definitive confirmation of AAV requires tissue diagnosis. The site of biopsy is an important determinant in the utility of the tissue specimen (see Table 1). Our patient underwent several sinus biopsies that yielded nonspecific results. This is not surprising, because a retrospective analysis of 158 patients with confirmed GPA demonstrated that nasal and sinus biopsies demonstrate vasculitis in less than 30% of patients, and even granulomas are seen in less than 60% of cases.3 In contrast, lung biopsy specimens from the same series demonstrated vasculitis in 87% and, indeed, the diagnosis in our case was confirmed with a lung biopsy. If there is evidence of renal involvement, a kidney biopsy may yield the diagnosis in over 95% of cases.4 An important consideration in interpreting renal biopsy results is whether the biopsy contains sufficient glomeruli, because the same series demonstrated that up to 40% of glomeruli from patients with GPA appeared normal on histology. The absence of an active urinary sediment suggested that our patient did not have significant glomerular involvement. Similarly, nerve biopsies have a relatively high diagnostic yield. A series of 83 patients with vasculitic neuropathy demonstrated that a nerve biopsy confirmed the diagnosis of vasculitis in 55% of patients, while a combined nerve and muscle biopsy increased the yield to 80% of patients.5
RB’s presentation, while in many ways classic for GPA, also had some atypical features. Specifically, genitourinary involvement is an uncommon presenting symptom in AAV, with only case reports describing prostatic, urethral, and penile involvement.6,7 However, an autopsy series done over 50 years ago demonstrated prostatic involvement in 7% of patients with GPA.8 Despite widespread systemic disease, he lacked any significant musculoskeletal symptoms, fevers, or rash. It has been reported that fewer than 70% of patients have prominent musculoskeletal complaints and less than a quarter of patients have skin disease at presentation.1,5
As demonstrated by this case, we must always be mindful of infection. While the vast majority of patients with AAV achieve remission following induction therapy with glucocorticoids and cyclophosphamide or rituximab, longer follow up suggests that the disease carries a 10% to 20% mortality with close to 25% of deaths attributable, at least in part, to infection.5,9
Take-Home Points
- ANCA testing is up to 96% sensitive in systemic AAV, but decreases in sensitivity with localized disease.
- Lung and renal biopsies, followed by combined nerve/muscle biopsy, have the highest diagnostic yield in systemic vasculitis, while sinus biopsies are often nondiagnostic.
- GPA should be considered in patients with atypical presentations of genitourinary disease.