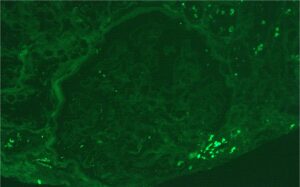
A renal biopsy was performed (see Figs. 1–3) and showed class 1 or class 2 lupus nephritis with diffuse podocyte foot process effacement and minimal mesangial immune complex deposition, consistent with lupus podocytopathy. replacement therapy was initiated in the hospital, and she remained dialysis dependent for approximately six weeks. A few days after dialysis was initiated, mycophenolate mofetil (MMF) was started to induce remission of her lupus podocytopathy. Later during her clinical course, she experienced gastrointestinal intolerance, so she was switched from MMF to mycophenolic acid (MPA). She was continued on hydroxychloroquine at a renally adjusted dose of 200 mg once daily.
Two months after her initial presentation, her proteinuria improved to a urine protein to creatinine ratio of 393 mg/g, and her renal function improved, with a creatinine level of 1.04 mg/dL and an eGFR of 52 mL/min/1.73 m2. A glucocorticoid taper was continued.
Four months after her initial diagnosis of lupus podocytopathy, while she was taking 30 mg of prednisone daily, hydroxychloroquine and MPA, she relapsed, experiencing worsening edema with a urine protein to creatinine ratio of 15,111 mg/g and deteriorating renal function, with a creatinine level of 2.8 mg/dL and eGFR of 22 mL/min/1.73 m2. Her prednisone dose was increased back to 60 mg per day and voclosporin, a novel calcineurin inhibitor (CNI), was added, renally dose adjusted to 7.9 mg twice a day.
About a month following this relapse (five months after diagnosis), MPA was discontinued due to worsening gastrointestinal side effects and intravenous cyclophosphamide was initiated in an attempt to induce remission. Her renal function continued to deteriorate, with peak creatinine of 4.96 mg/dL, eGFR 9 mL/min/1.73 m2 and a urine protein to creatinine ratio of 29,569 mg/g. Diureticrefractory edema and symptomatic uremia necessitated re-initiation of renal replacement therapy.
A repeat renal biopsy (see Figure 4) showed focal segmental glomerulosclerosis (FSGS), diffuse podocyte foot process effacement and low intensity mesangial immune deposits consistent with mesangial lupus nephritis (class 1) and lupus podocytopathy. She continued a regimen of monthly, intravenous cyclophosphamide, hydroxychloroquine, low-dose voclosporin and slow taper of prednisone. After completion of six monthly doses of intravenous cyclophosphamide, the patient’s renal function improved to an eGFR of 35 mL/min/1.73 m2, creatinine of 1.5 mg/dL and a 24-hour proteinuria of 480 mg. Thus, dialysis was discontinued. The prednisone dose was tapered slowly to 6 mg daily, with plans to continue tapering at the last follow up, which was 16 months following the initial diagnosis of lupus podocytopathy. Rituximab maintenance therapy was initiated at two doses of 1 g each at two-week intervals, with the intention of continuing her treatment with 1 g every six months thereafter.