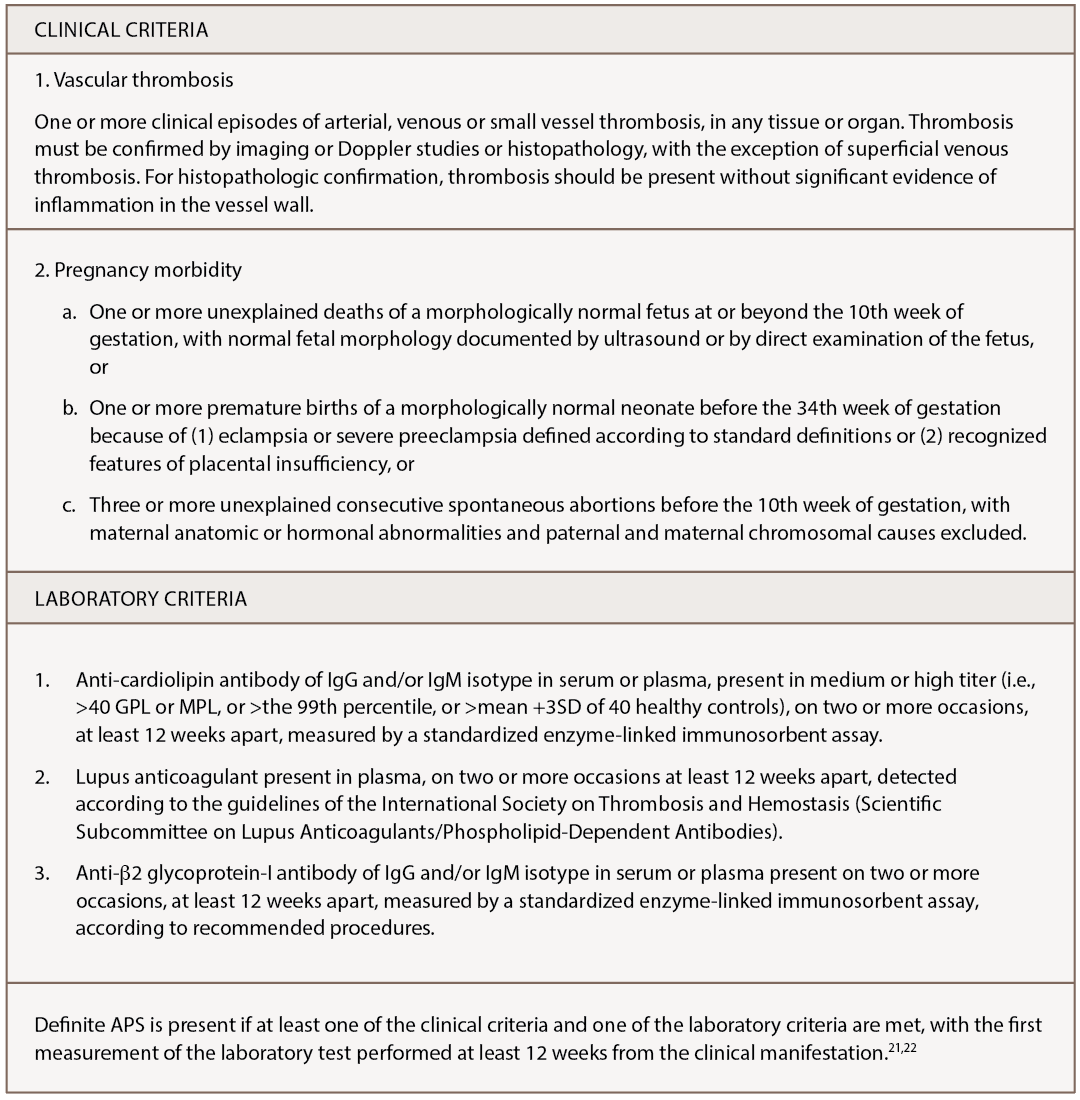
Of note, however, not every positive antiphospholipid antibody (aPLA) is clinically significant, and not every patient with positive aPLA has the same risk. Other factors, such as cardiovascular disease and recent trauma, play a role. A clinically significant anti-cardiolipin antibody greater than or equal to 40 units or anti-β2 glycoprotein-I antibody greater than or equal to 40 units is tested twice at least 12 weeks apart.23 Further, a positive lupus anticoagulant test is based on guidelines from the International Society of Thrombosis and Haemostasis.21
Buddha Basnyat, MD, and colleagues describe a young man with APS who experienced vision changes and abdominal pain while climbing at 7,000 meters in the Himalayas.24 The patient was found to have superior mesenteric vein thrombosis, as well as multiple venous sinus thromboses.
Another study of 20 volunteers on a flight from Vienna to Washington demonstrates an increased activity of clotting factor VII and VIII, suppressed fibrinolysis and reduced activated partial thromboplastin time (aPTT) measurements after the flight.25
A study of six climbers traveling in the Argentinian Andes up Aconcagua, the highest peak in South America, to an altitude of greater than 6,000 meters in 2007, found that all of them had retinal vascular engorgement and tortuosity after the climb.26 Of the two who experienced visual changes, one had an elevated aPLA. Since that report was published, ophthalmologists recommend individuals with glaucoma, age-related macular degeneration or diabetic retinopathy avoid prolonged and unnecessary high-altitude exposure without appropriate acclimatization.11
Guidelines specific to APS, travel & long-haul flights are lacking. The protective effect of low dose aspirin in individuals with clinically significant aPLA values is not supported by randomized controlled data.
Guidelines from Professional Societies
Guidelines specific to APS, travel and long-haul flights are lacking. The protective effect of low dose aspirin (ASA) in individuals with clinically significant aPLA values is not supported by randomized controlled data. Moreover, little evidence exists showing that aspirin is of great benefit for high-risk individuals while traveling. However, Maria Cesarone, MD, and colleagues concluded that enoxaparin (1 mg/kg) administered two to four hours before traveling may minimize the risk of DVT.27
Further risk stratification based on aPLA profile, age, concomitant systemic autoimmune disease and cardiovascular disease categorizes an individual to low-, moderate- or high-risk categories.20 Individuals with no medical conditions traveling fewer than eight hours or fewer than 5,000 kilometers are at low risk. Moderate-risk patients include those who are obese, pregnant, on hormone-replacement therapy or oral contraceptives, or who use tobacco and have longer travel times and distances. High-risk patients may have a history of VTE, hypercoagulable state, recent surgery or malignancy.