In the LONFLIT3 study, three high-risk groups were studied: One was given no prophylaxis, one was given ASA, and the last received low-molecular-weight heparin (LMWH; enoxaparin).27 Results revealed the group given enoxaparin developed no DVT, whereas several individuals in the other two groups did develop DVT. Several years later, the American College of Chest Physicians (ACCP) devised recommendations for those considered at high risk of VTE, which includes individuals with APS (see Table 2).28 In addition to recommending general measures for those at a low risk of clotting (e.g., minimize constrictive clothing, maximize hydration and carry out frequent calf muscle exercises [Grade 1C]), the ACCP suggests below-the-knee graduated compression stockings (Grade 2C) or a single dose of LMWH prior to flight (Grade 2C). It does not support the use of ASA for VTE prophylaxis (Grade 1B).28
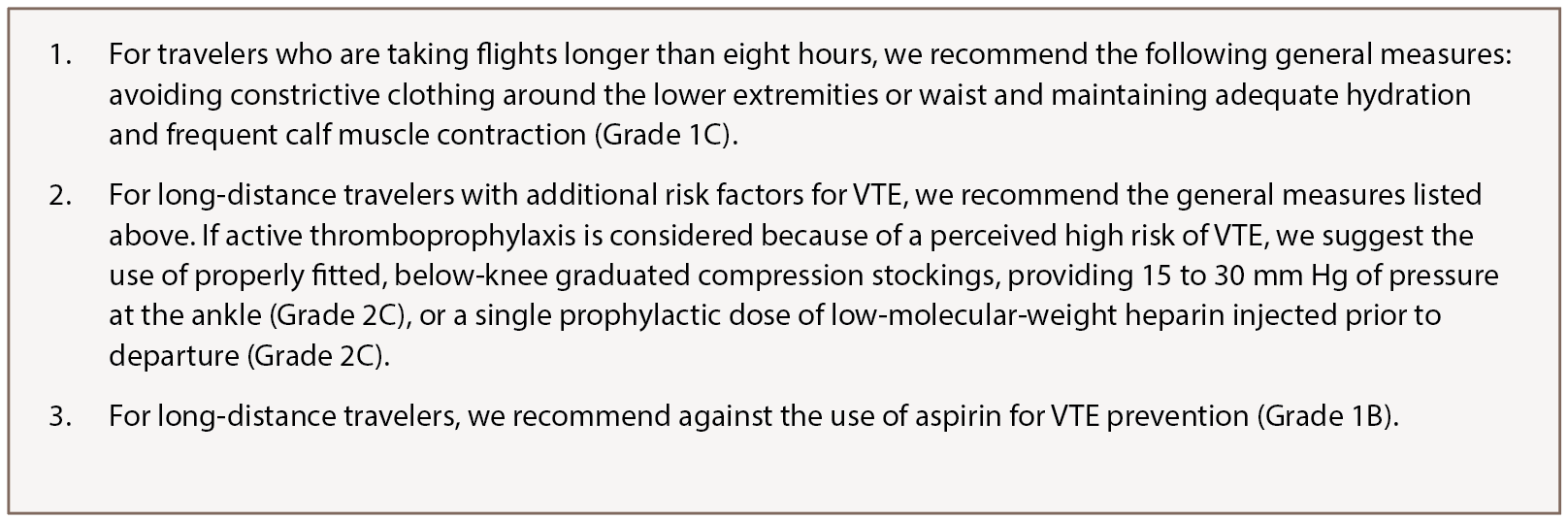
(click for larger image) Table 2: American College of Chest Physicians Long-Distance Travel Recommendations28
Authors’ Conclusions & Recommendations
It is prudent for practitioners to consider anticoagulation for high-risk patients with APS who are traveling for long distances or at high altitudes. When deciding whether to anticoagulate a patient positive for aPLA, it is important to be attentive of clinically significant laboratory values, as well as comorbidities associated with a greater increase in the risk of clotting. Further, in individuals with known APS, consideration for a booster dose of enoxaparin (1 mg/kg) is not unreasonable two to four hours prior to travel on flights exceeding eight hours’ duration. Although our recommendations are based on a review of the literature, further research is encouraged for patients with APS to assist in preventive measures and overall improved quality of life.
Vaneet Kaur Sandhu, MD, is an assistant professor in the Division of Rheumatology at Loma Linda University, Loma Linda, Calif.
Kathleen Teves, MD, is an internal medicine resident at the University of California, Riverside, Calif.
References
- Anderson FA Jr., Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003 Jun 17;107(23 Suppl1):I9–I11.
- Anand AC, Saha A, Seth AK, et al. Symptomatic portal system thrombosis in soldiers due to extended stay at extreme altitude. J Gastroenterol Hepatol 2005 May;20(5):777–783.
- Auerbach PS. Wilderness Medicine, 5th ed. Philadelphia: Mosby, 2007.
- Bärtsch P. How thrombogenic is hypoxia? JAMA. 2006 May 17;295(19):2297–2299.
- Yan SF, Mackman N, Kisiel W, et al. Hypoxia/hypoxemia-induced activation of the procoagulant pathways and the pathogenesis of ischemia-associated thrombosis. Arterioscler Thromb Vasc Biol. 1999 Sep;19(2):2029–2035.
- Ninivaggi M, de Laat M, Lancé MM, et al. Hypoxia induces a prothrombotic state independently of the physical activity. PLoS ONE. 2015 Oct 30;10(10):e0141797.
- Cannegieter SC, Doggen CJ, van Houwelingen HC, et al. Travel-related venous thrombosis: Results from a large population-based case control study (MEGA study). PLoS Med. 2006 Aug;3(8):e307.
- Kraaijenhagen RA, Haverkamp D, Koopman MM, et al. Travel and risk of venous thrombosis. Lancet. 2000 Oct 28;356(9240):1492–1493.
- Ferrari E, Chevallier T, Chapelier A, et al. Travel as a risk factor for venous thromboembolic disease: A case-control study. Chest. 1999 Feb;115(2):440–444.
- Rosendaal FR. Interventions to prevent venous thrombosis after air travel: Are they necessary? No. J Thromb Haemost. 2006 Nov;4(11):2306–2307.
- Georgalas I. Climbing the Himalayas more safely BMJ. 2012 Jun 13;344:e3778.
- Hoeper MM, Granton J. Intensive care unit management of patients with severe pulmonary hypertension and right heart failure. Am J Respir Crit Care Med. 2011 Nov 15;184(10):1114–1124.
- Bradford A. The role of hypoxia and platelets in air travel-related venous thromboembolism. Curr Pharm Des. 2007;13(26):2668–2672.
- Martin DS, Pate JS, Vercueil A, et al. Reduced coagulation at high altitude identified by thromboelastography. Thromb Haemost. 2012 Jun;107(6):1066–1071.
- Sabit R, Thomas P, Shale DJ, et al. The effects of hypoxia on markers of coagulation and systemic inflammation in patients with COPD. Chest. 2010 Jul;138(1):47–51.
- Schreijer AJ, Cannegieter SC, Doggen CJ, et al. The effect of flight-related behaviour on the risk of venous thrombosis after air travel. Br J Haematol. 2009 Feb;144(3):425–429.
- Toff WD, Jones CI, Ford I, et al. Effect of hypobaric hypoxia, simulating conditions during long-haul air travel, on coagulation, fibrinolysis, platelet function, and endothelial activation. JAMA. 2006 May 17;295(19):2251–2261.
- Kuipers S, Schreijer AJM, Cannegieter SC, et al. The absolute risk of venous thrombosis after air travel (WRIGHT study). J Thromb Haemost. 2005;3:P1657.
- Aldington S, Pritchard A, Perrin K, et al. Prolonged seated immobility at work is a common risk factor for venous thromboembolism leading to hospital admission. Int Med J. 2008 Feb;38(2):133–135.
- Silverman D, Gendreau M. Medical issues associated with commercial flights. Lancet. 2009 Jun 13;373(9680):2067–2077.
- Miyakis S, Lockshin MD, Atsumi T, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. 2006 Feb;4(2):295–306.
- Gómez-Puerta JA, Cervera R. Diagnosis and classification of the antiphospholipid syndrome. J Autoimmun. 2014 Feb–Mar;48–49:20–25.
- Barbhaiya M, Erkan D. Primary thrombosis prophylaxis in antiphospholipid antibody-positive patients: Where do we stand? Curr Rheumatol Rep. 2011 Feb;13(1):59–69.
- Basnyat B, Graham L, Lee SD, et al. A language barrier, abdominal pain, and double vision. Lancet. 2001 Jun 23;357(9273):2022.
- Schobersberger W, Fries D, Mittermayr M, et al. Changes of biochemical markers and functional tests for clot formation during long-haul flights. Thromb Res. 2002 Oct 1;108(1):19–24.
- Ho TY, Kao WF, Lee SM, et al. High-altitude retinopathy after climbing Mount Aconcagua in a group of experienced climbers. Retina. 2011 Sep;31(8):1650–1655.
- Cesarone MR, Becaro G, Nicolaides AN, et al. Venous thrombosis from air travel: The LONGFLIT3 study—Prevention with aspirin vs low-molecular-weight heparin (LMWH) in high-risk subjects: A randomized trial. Angiology. 2002 Jan–Feb;53(1):1–6.
- Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest. 2008 Jun;133(6 Suppl):381S–453S.
