Making a definitive CPPD diagnosis in symptomatic cases often requires arthrocentesis, or aspirating the affected joint and examining its synovial fluid under microscopy for the presence of calcium pyrophosphate crystals.
“If you’re not used to looking at these crystals, finding them can be very challenging,” Dr. Rosenthal says. Gout crystals are large, needle-shaped, sharply defined, usually abundant and easy to see under polarizing light. Rod and rhomboid-shaped calcium pyrophosphate crystals, by contrast, are fuzzy around the edges, far smaller and much less bright under polarizing light.
Fortunately, Dr. Rosenthal says better imaging techniques, including ultrasound and computed tomography-based methods, are expanding diagnostic capabilities. “My hope for the future is that although we still should rely on synovial fluid analysis, there may be less invasive forms of confirming a diagnosis in a lot of these patients,” she says.
More sophisticated computational techniques may aid microscopy-based diagnostics as well. “Those are really exciting because I think we’re missing a lot of it,” Dr. Rosenthal says. “There are people that are misdiagnosed or just ignored.”
With better diagnostics, she says, the field could come closer to launching clinical trials of therapies that target inflammation, as well as crystal formation and development.
Acute Pseudogout Presentation
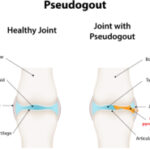
Of the symptomatic forms of CPPD, one of the most common is widely known as pseudogout, acute CPPD or, officially, acute CPP crystal arthritis.
“It’s like a stroke of lightning where all of a sudden, the patient who was normal the day before wakes up and they have an acutely inflamed knee that they can hardly stand on because it hurts so bad,” Dr. Bettendorf says. “Often, the joint will be swollen, hot, red and we would, in that case, end up taking fluid out of the joint to look for crystals and make the diagnosis.”
Roughly half of initial gout attacks occur in the big toe, Dr. Baraf says; whereas pseudogout most commonly impacts other joints, especially the knee. “The big toe is to gout as the knee is to pseudogout,” he says. Pseudogout also commonly affects the wrist, although it can instead flare in a shoulder, hand or ankle joint. The sudden onset can occasionally follow surgery, he notes, such as resection of the parathyroid gland.
“It looks very much like true gout, and for years it was probably misdiagnosed until we really started using polarizing microscopy to make that differentiation between gout and pseudogout,” Dr. Rosenthal says. The abrupt clinical presentation plus imaging and microscopy have now greatly aided the diagnosis. “The most recognizable clinical manifestation is the flare-up, and the easiest to prove with X-ray and synovial fluid crystal examination,” Dr. Baraf says. “If you get all that together, you have an airtight case.” For some patients, imaging has revealed both gout and pseudogout crystals.