Chronic Presentations
Another common form of CPPD is a chronic osteoarthritis (OA) like presentation. “It’s fairly non-inflammatory arthritis affecting joints that are not typically affected by garden-variety osteoarthritis,” Dr. Rosenthal says. Beyond the knee, CPPD disease can affect the shoulder, elbow, wrist and ankle joints, for example. In the hands, the presentation can be a relatively distinct form of arthritis that involves the second and third metacarpophalangeal joints.
The symptoms generally don’t include systemic issues like a low-grade fever. “Maybe the patient has chronically sore hands, where they’re noticing they have difficulty opening bottles or turning door handles; they’re noticing maybe that their grip is weaker,” Dr. Bettendorf says. “Their hands are stiff and sore more in the mornings and take a while to loosen up.” She also sees CPPD in joints in which advanced OA has worn down the cartilage, primarily in older patients. Called osteoarthritis with CPPD, that form tends to appear most commonly in the hip and knee joints.
Dr. Rosenthal says she generally treats her CPPD patients with an OA-like presentation similarly to how she would treat true OA. She often starts with an NSAID if the patient doesn’t have a contraindication, such as a kidney problem. She also uses intra-articular corticosteroids for amenable joints. “I think that’s a really interesting and effective, though temporary, fix,” she says.
Low-dose colchicine is another option used less often for true OA, and in some patients, Dr. Rosenthal has had success with low-dose parenteral or oral corticosteroids, such as prednisone (less than 10 mg per day).
Less commonly, CPPD disease can appear as a chronic rheumatoid arthritis-like condition that affects multiple joints and causes substantial inflammation. Officially known as chronic CPP crystal inflammatory arthritis, Dr. Bettendorf sometimes calls this form “pseudo-rheumatoid arthritis,” given its similarities and tendency to attack the same joints. Even so, she says, a good clinical workup can provide clues that differentiate inflammatory CPPD, including a lack of antibodies for rheumatoid arthritis.
“It’s good to keep this at the back of our minds when we are evaluating patients for what seems to be typical inflammatory arthritis, like rheumatoid arthritis,” adds Dr. Bose. “Sometimes chronic CPPD may appear as rheumatoid arthritis, [but] it just won’t have the markers and none of the radiographic changes.”
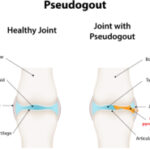
Unlike the propensity of rheumatoid arthritis to impact other organs, CPPD disease is generally limited to a patient’s joints and cartilage. “CPPD won’t cause pericardial effusion around the heart or lung disease, which could happen with rheumatoid arthritis,” Dr. Bettendorf says.