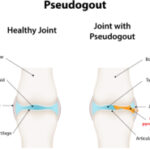
In addition, imaging can reveal evidence of bulky bone spurs on the metacarpals of the hand and chondrocalcinosis in cartilage, such as the triangular fibrocartilage complex of the wrist. Dr. Bettendorf cautions, however, that chondrocalcinosis can appear in a patient who has never had any signs or symptoms of CPPD, like the asymptomatic older patients in the 1975 study, meaning that imaging alone isn’t always sufficient for a diagnosis. “I think about it as one piece of the puzzle, but really what we need is that fluid from around the joint and making sure that we confirm the correct diagnosis,” she says.
Here too, treatment options have been steadily expanding. “For this chronic inflammatory type, we use the same drugs as we use for osteoarthritislike phenotypes, but in higher doses,” Dr. Rosenthal says.
Colchicine has worked well for treating some of Dr. Bettendorf’s patients. As with rheumatoid arthritis, doctors have also administered disease-modifying anti-rheumatic drugs (DMARDs), such as methotrexate and hydroxychloroquine, although with more variable results. Some have experimented with drug combinations that include prednisone and colchicine. Limited evidence has suggested IL-6 inhibitors and IL-1 beta inhibitors used to treat rheumatoid arthritis may have utility here as well.
Rarities & Risk Factors
In rare cases, Dr. Rosenthal says, CPPD can resemble neuroarthropathy, which involves a sensory nerve abnormality that causes a loss of sensation and extensive joint damage, most often in the ankle or foot. Alternatively, the crystal deposition can be in a tophus-like or cluster-like formation within the body’s soft tissue, giving it the appearance of a tumor.
Dr. Bettendorf has even seen CPPD cases involving the temporomandibular joint, which attaches the lower jaw to the skull, or the odontoid process of the cervical spine, where ligaments attach to the upper portion of the spinal column.
“When that happens, it can actually have a pseudo-meningitis type of presentation, [in which] somebody might have low-grade fevers, difficulty moving their head or their neck, and severe pain with that—and it looks, for all the world, like meningitis,” says Dr. Bettendorf. A negative spinal tap, however, can prompt doctors to order imaging that reveals calcium pyrophosphate crystals surrounding the odontoid process. “When that happens, that can be a scarier presentation, but it’s something that we can treat.”
Although CPPD’s etiology and the mechanisms leading to its many forms remain uncertain, researchers have identified four main classes of risk factors. First, advanced age increases the risk for the sporadic form of the disease. Second, four metabolic diseases that result in the mishandling of pyrophosphate can also increase risk. Dr. Rosenthal calls them the four Hs: hemochromatosis (excess iron absorption), hypophosphatasia (low levels of alkaline phosphatase), hypomagnesemia (low magnesium levels), and hyperparathyroidism (excess parathyroid hormone). A fifth condition, hypothyroidism, was once thought to be associated as well, but research now suggests it is not.